Table of Contents
How Head Injuries Affect Mobility & Flexibility—and How Integrative, Chiropractic-Led Care Helps You Recover

Key Takeaways
-
Head injuries (traumatic brain injuries, or TBIs) can cause muscle fatigue, poor coordination, balance problems, slower walking, and—at the severe end—partial or complete paralysis. These issues often worsen when you’re tired or in pain (Headway, n.d.; MSKTC, n.d.). Headway+1
-
Immobility after a head injury can lead to muscle tightening and joint stiffness (contractures), reducing overall flexibility if not managed early (Physiopedia, n.d.; NR Times, 2023). Physiopedia+1
-
Physical therapy leverages neuroplasticity—your brain’s ability to adapt—to restore function, balance, and gait (BIAUSA, n.d.). Brain Injury Association of America
-
Chiropractic and integrative care—spinal adjustments, soft-tissue therapy, vestibular and vision drills, and graded exercise—can help realign joints, reduce soft-tissue tension, improve proprioception, and support the nervous system’s recovery, especially when the neck is involved (CognitiveFX, 2025; MSKTC, n.d.; Dr. Alex Jimenez, n.d.). Cognitive FX+2MSKTC+2
Why Head Injuries Change the Way You Move
A head injury can disrupt the brain’s motor networks (cortex, brainstem pathways, basal ganglia, cerebellum). That disruption manifests as weakness (paresis), spasticity, slowed movement (hypokinesia), tremors, poor coordination (ataxia), and balance problems. These changes limit walking speed, stride length, and the ability to start, stop, or turn smoothly (Moon, 2022; Row et al., 2019). PMC+1
-
Fatigue multiplies symptoms. Many people with TBI report heavy physical and mental fatigue; it’s one of the most common long-term complaints, and it makes mobility worse (MSKTC, n.d.). MSKTC
-
“Small” changes matter. Even subtle shifts in gait and balance can significantly impact daily life and safety (BIAUSA, n.d.). Brain Injury Association of America
-
Neck involvement is common. After concussions or crash-related head/neck trauma, neck pain and cervicogenic dizziness can limit range of motion and alter balance and posture (CognitiveFX, 2024). Cognitive FX
Bottom line: Head injuries alter signals between your brain, nerves, and muscles. When those signals are noisy or delayed, you experience stiffness, poor timing, and compensations that sap mobility and flexibility (Headway, n.d.; Brain Injury Canada, n.d.). Headway+1
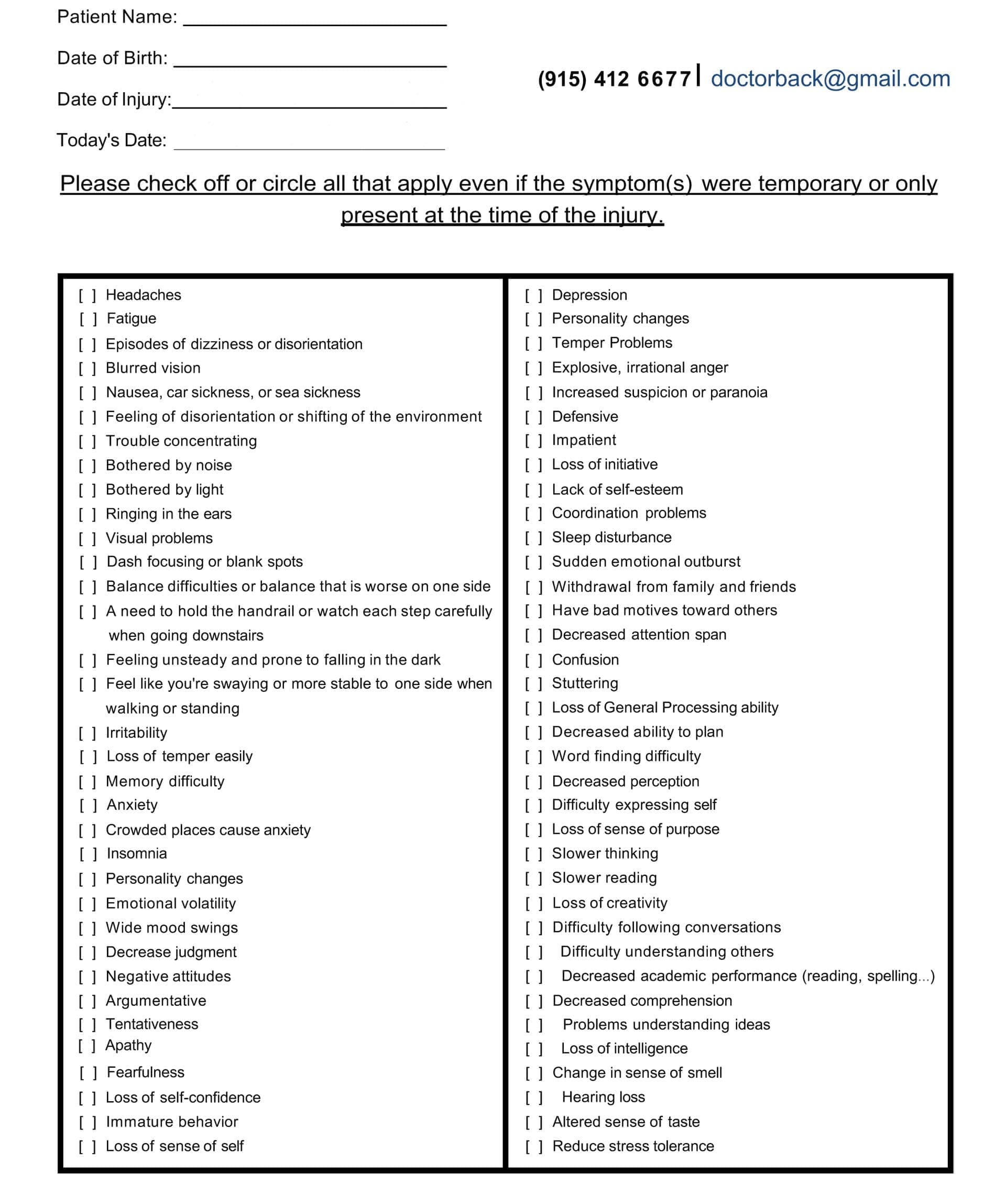
Symptom Questionnaire:
From Immobility to Contractures: How Flexibility Declines
When movement is painful, weak, or poorly coordinated, people naturally move less. Less movement ? shortened muscles and tighter connective tissues ? contractures that restrict joints and reduce flexibility. Without early management (stretching, positioning, splinting, and guided mobility exercises), contractures can develop and become difficult to reverse (Physiopedia, n.d.; NR Times, 2023). Physiopedia+1
Contributors to contractures after head injury
-
Spasticity and hypertonicity
-
Weakness and disuse
-
Poor postural control and asymmetry
-
Pain that limits activity (Clinical Pain Advisor, 2017; Curran et al., 2024). Clinical Pain Advisor+1
Common Mobility & Balance Problems You Might Notice
-
Slow or effortful walking; shorter steps; feeling “off” with turns (Headway, 2025 PDF). Headway
-
Unsteadiness and falls, especially when multitasking or in busy visual environments (MSKTC, n.d.). MSKTC
-
Poor single-leg stance; difficulty with stairs or uneven ground (BIAUSA, n.d.). Brain Injury Association of America
-
Neck stiffness and headaches that change posture and shoulder mechanics (CognitiveFX, 2024). Cognitive FX
Even if your MRI is “normal,” post-TBI balance testing often reveals meaningful deficits that explain your symptoms and guide treatment (BIAUSA, n.d.). Brain Injury Association of America
How Rehabilitation Helps: The Science of Neuroplasticity
Neuroplasticity is your brain’s capacity to rewire with targeted practice. Physical therapy and related neuro-rehab techniques use graded, meaningful tasks to restore coordination, strength, and balance. Programs progress from basic to complex tasks, often pairing aerobic exercise with task-specific practice for better brain outcomes (BIAUSA, n.d.; Gómez-Pinilla, 2022). Brain Injury Association of America+1
Core goals after a head injury
-
Re-establish safe walking and transfers
-
Improve balance and reduce falls
-
Normalize movement patterns and posture
-
Restore endurance so fatigue doesn’t trigger setbacks (BIAUSA, n.d.; MSKTC, n.d.). Brain Injury Association of America+1
Where Chiropractic & Integrative Care Fit
An integrative plan combines conventional rehabilitation with chiropractic care, soft-tissue therapies, vestibular/vision exercises, breathing techniques, and progressive strength/aerobic training. This whole-person approach aims to realign joints, reduce muscle guarding, improve joint glide and proprioception, and support normal sensorimotor signaling between the neck, spine, and brain (CognitiveFX, 2025; MSKTC, n.d.). Cognitive FX+1
Typical elements
-
Spinal and regional joint adjustments/mobilization to address restricted segments that alter mechanics and loading.
-
Soft-tissue therapy (manual release, instrument-assisted, neuromuscular techniques) for overactive or shortened tissues.
-
Vestibular and oculomotor drills to recalibrate balance systems.
-
Targeted strength and gait training to restore symmetry and endurance.
-
Breathing and autonomic regulation to reduce dizziness and exercise intolerance.
-
Lifestyle coaching (sleep, anti-inflammatory nutrition, activity pacing) to limit flare-ups (CognitiveFX, 2023–2025; Dr. Alex Jimenez, n.d.). Cognitive FX+2Cognitive FX+2
Clinical perspective — Dr. Alexander Jimenez, DC, APRN, FNP-BC (El Paso)
In practice, patients with head injuries often carry cervical and upper-thoracic restrictions that drive abnormal posture, shoulder elevation, and headaches. Dr. Jimenez’s integrated approach prioritizes restoring cervical mobility, scapular control, and deep neck flexor strength while layering vestibular drills and graded walking. Many patients report smoother gaze, steadier footing, and less “neck-triggered dizziness” as alignment and soft-tissue tone normalize (Dr. Alex Jimenez, n.d.). El Paso, TX Doctor Of Chiropractic+1
Note: Some clinic websites also report improved circulation and symptom relief with chiropractic care; while encouraging, these claims should be considered adjunctive and individualized (selected clinic sources). El Paso Back Clinic® • 915-850-0900
Step-by-Step: A Gentle Return-to-Mobility Plan
Always clear red flags (worsening neuro signs, severe headache, new weakness, fainting, or suspected cervical instability) with a licensed clinician.
Phase A — Calm the System & Re-establish Range (Days 1–21)
-
Daily mobility breaks (3–5×/day, 5–10 min):
-
Chin nods ? cervical rotations (pain-free arc), thoracic extensions over a towel roll, scapular sets.
-
Long-exhale breathing (1:2 inhale: exhale) for autonomic calm.
-
-
Gentle vestibular basics: VOR x1 gaze stabilization at a comfortable speed (stop if symptoms spike).
-
Walking “snacks”: 5–10 minutes on flat ground; increase only if symptoms stay ?3/10 and resolve within an hour (MSKTC, n.d.). MSKTC
-
Positioning to prevent contractures: Neutral joint positions, supported sitting posture, and frequent change-of-position (Physiopedia, n.d.; NR Times, 2023). Physiopedia+1
-
Manual care (clinic): Spinal and rib mobilization; soft-tissue release of suboccipitals, levator scapulae, scalenes, and pectorals as tolerated (CognitiveFX, 2025; Dr. Alex Jimenez, n.d.). Cognitive FX+1
Phase B — Build Stability, Balance & Endurance (Weeks 3–8)
-
Strength (3×/week):
-
Glute bridge, sit-to-stand, supported split squat, row or band pull-apart, dead bug or bird dog.
-
-
Balance ladder:
-
Feet together ? semi-tandem ? tandem stance ? single-leg stance (near support).
-
Add head turns and eyes-closed variations as tolerated (MSKTC, n.d.; BIAUSA, n.d.). MSKTC+1
-
-
Aerobic progression: 20–40 min at easy-moderate effort (RPE 11–13). Evidence supports the regular practice of exercise to enhance cognitive and emotional outcomes following TBI (Gómez-Pinilla, 2022). PMC
-
Gait quality: Cue upright posture, arm swing, and even step length; practice small-space turns and dual-task walking (BIAUSA, n.d.). Brain Injury Association of America
Phase C — Power, Agility & Real-Life Tasks (Weeks 8–16+)
-
Task specificity: Curb negotiation, stair patterns, carrying groceries, uneven surfaces.
-
Light agility: Lateral steps, retro-walking, gentle change-of-direction drills.
-
Return-to-work/leisure with symptom-aware pacing and recovery days (BIAUSA, n.d.; MSKTC, n.d.). Brain Injury Association of America+1
Smarter Flexibility: Preventing (and Reversing) Stiffness
-
Daily mobility circuit (10–15 min): Thoracic opener, wall angels, hip flexor and calf stretch, hamstring “sliders,” shoulder CARs, and gentle neck range.
-
Contracture prevention: Timed stretches (30–60 s), splinting/positioning, active-assist range, and early mobilization (Physiopedia, n.d.). Physiopedia
-
Soft-tissue + joint care: Manual therapy eases tone; adjustments/mobilization restore joint play so muscles don’t keep fighting a “stuck” segment (CognitiveFX, 2025; Dr. Alex Jimenez, n.d.). Cognitive FX+1
The Neck–Balance–Headache Triangle
Neck dysfunction can create or worsen dizziness, headaches, blurred vision, and imbalance. Addressing cervical alignment and motor control, including deep neck flexor activation, scapular stability, and graded mobility, often unlocks progress in balance and gait (CognitiveFX, 2024; MSKTC, n.d.). Cognitive FX+1
Clinic example (integrative approach):
-
Cervical/thoracic mobilization ? 2) soft-tissue release ? 3) gaze stabilization (VOR) ? 4) balance ladder ? 5) gait-quality cues. Patients commonly report less head “heaviness,” fewer headaches, and steadier walking as these pieces align (Dr. Alex Jimenez, n.d.). El Paso, TX Doctor Of Chiropractic
Safety First: Red Flags & When to Re-Evaluate
Seek urgent medical care if you have:
-
New weakness or numbness; new slurred speech; fainting or seizures
-
A severe, worsening headache; repeated vomiting
-
Sudden vision loss or double vision; neck pain that is severe and unrelenting
If your walking, balance, or flexibility plateau or worsens despite practice—or if small tasks cause big symptom spikes—request a comprehensive balance/vestibular evaluation; even subtle deficits can be identified and treated (BIAUSA, n.d.). Brain Injury Association of America
Putting It All Together: A Sample Week
Mon/Wed/Fri (Strength + Balance, ~40–60 min)
-
Warm-up mobility (10 min) ? lifts (20 min) ? balance ladder (10 min) ? gaze drills (5 min) ? breathing down-shift (5 min).
Tue/Thu/Sat (Aerobic + Gait, 20–40 min) -
Easy walk or cycle ? posture/arm-swing cues ? short dual-task segments (count backwards, name categories while walking).
Daily (2–3 “movement snacks”) -
Neck/shoulder ROM, hip flexor + calf stretch, thoracic openers; brief mindfulness or box breathing.
Weekly care (as prescribed) -
Chiropractic adjustments/mobilization; soft-tissue therapy; PT/vestibular visits; progression checks (BIAUSA, n.d.; CognitiveFX, 2023–2025). Brain Injury Association of America+1
What Progress Looks Like
-
Longer walking time before fatigue
-
Fewer stumbles and steadier turns
-
Improved neck rotation and upright posture
-
Better tolerance for household and community tasks
-
Shorter “recovery time” after activity (MSKTC, n.d.; BIAUSA, n.d.). MSKTC+1
Even small wins compound. Evidence and clinical experience agree: consistent, well-paced practice rebuilds function after head injuries (BIAUSA, n.d.; Gómez-Pinilla, 2022; Row et al., 2019). Brain Injury Association of America+2PMC+2
Final Word
Head injuries can lower mobility and flexibility by tightening muscles, stiffening joints, and disrupting nerve signals—especially when the neck is involved. The path back combines neuro-informed rehabilitation and integrative chiropractic care, restoring alignment and joint motion, reducing soft-tissue guarding, retraining balance and gaze control, and building endurance through smart pacing. With consistent practice and a personalized plan, most people see steady, meaningful gains in walking, stability, and range of motion (BIAUSA, n.d.; MSKTC, n.d.). Brain Injury Association of America+1
References
-
Brain Injury Association of America. (n.d.). Physical therapy and brain injury recovery. biausa.org/ Brain Injury Association of America
-
Brain Injury Association of America. (n.d.). Brain injury rehabilitation. biausa.org/ Brain Injury Association of America
-
Brain Injury Association of America. (n.d.). Slight changes in walking and balance after traumatic brain injury. biausa.org/ Brain Injury Association of America
-
Brain Injury Association of America. (n.d.). Factors associated with sitting and standing balance. biausa.org/ Brain Injury Association of America
-
Brain Injury Canada. (n.d.). Traumatic brain injury—Physical changes & mobility challenges. braininjurycanada.ca/ Brain Injury Canada
-
Cognitive FX. (2025, Jan 24). A patient’s guide to TBI physical therapy. www.cognitivefxusa.com/ Cognitive FX
-
Cognitive FX. (2024, Jun 28). Post-concussion syndrome neck pain. www.cognitivefxusa.com/ Cognitive FX
-
Cognitive FX. (2023, Apr 5). Physical therapy for post-concussion syndrome. www.cognitivefxusa.com/ Cognitive FX
-
Gómez-Pinilla, F. (2022). How to boost the effects of exercise to favor traumatic brain injury repair. Frontiers in Neuroscience. pmc.ncbi.nlm.nih.gov/ PMC
-
Headway – the brain injury association. (n.d.). Physical effects of brain injury (Mobility & movement problems). www.headway.org.uk/ Headway
-
Headway – the brain injury association. (2025). The effects of brain injury [PDF]. www.headway.org.uk/ Headway
-
MSKTC. (n.d.). Understanding TBI, Part 2: How a TBI affects thinking and functioning. msktc.org/ MSKTC
-
MSKTC. (n.d.). Balance problems after traumatic brain injury (fact sheet & infographic). msktc.org/ MSKTC+1
-
MSKTC. (n.d.). Fatigue after TBI. msktc.org/ MSKTC
-
Moon, D., et al. (2022). Disorders of movement due to acquired and traumatic brain injury. Frontiers in Neurology. pmc.ncbi.nlm.nih.gov/ PMC
-
NR Times. (2023). Physiotherapy in post-TBI rehab (overview on joint stiffness/contracture prevention). nrtimes.co.uk/ NCBI
-
Physiopedia. (n.d.). Contracture management for traumatic brain injury. www.physio-pedia.com/ Physiopedia
-
Row, J., et al. (2019). Balance assessment in traumatic brain injury. Journal of NeuroEngineering and Rehabilitation. pmc.ncbi.nlm.nih.gov/ PMC
-
Curran, M. C., et al. (2024). Chronic pain after traumatic brain injury: A collaborative perspective. pmc.ncbi.nlm.nih.gov/ PMC
-
Clinical Pain Advisor. (2017). Chronic pain associated with TBI. www.clinicalpainadvisor.com/ Clinical Pain Advisor
-
The Crumley House. (2025, Feb 5). How physical training supports TBI recovery. crumleyhouse.com/ crumleyhouse.com
-
Dr. Alex Jimenez. (n.d.). Clinic overview; mobility & flexibility resources. dralexjimenez.com/ El Paso, TX Doctor Of Chiropractic+1
Disclaimers
Professional Scope of Practice *
The information herein on "Head Injuries Affect Mobility & Flexibility: What to Know" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's wellness blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-C) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on dralexjimenez.com, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card