We have found that approaching the body as a whole rather than treating it as compartments gives patients the most relief. This is due to the fact that we are not band-aiding symptoms, but treating the issue at its cause. As research develops, it is found that over 125 clinical conditions have been identified as having inflammation along with oxidative stress as a contributing factor to the diagnosis.Â
Table of Contents
Inflammation Part 1
The nervous system and the immune system are closely intertwined. If there is an abnormality with one, the other will be affected. Neurological symptoms include fatigue, poor mood, cognitive impairment, and lack of motivation whereas immune symptoms involve being sick in general or cold/flu-like symptoms. These symptoms are not the problem, but rather a reaction to what is happening further down in the body systems. When inflammation is present, it will always affect all other symptoms of the body. With inflammation, we are quick to see oxidative stress follow.Â
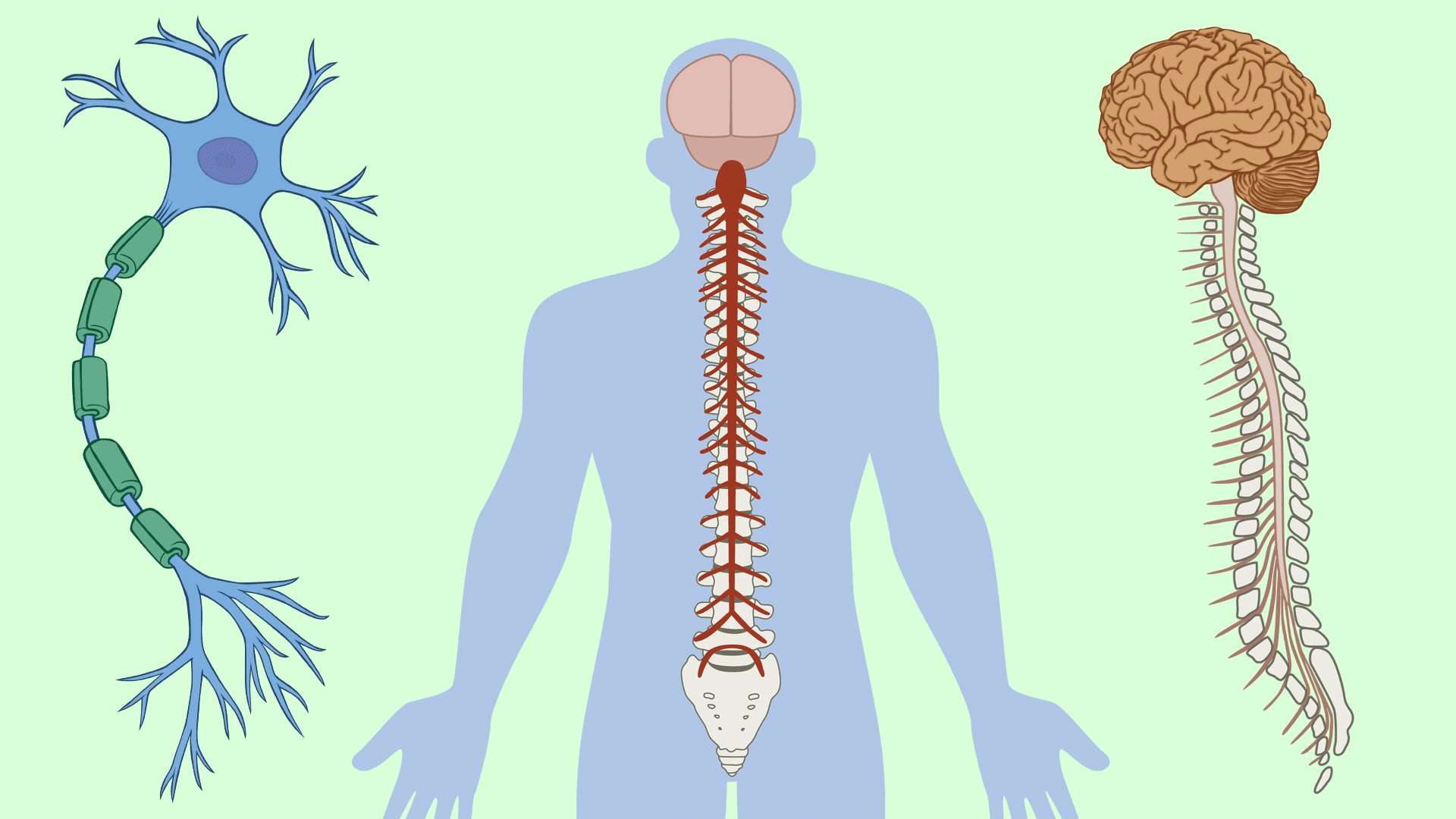
The Nervous System
When looking at the nervous system, we see that neurotransmitters and neuropeptides are in the immune system, leading researchers to study if our immunity is primarily nerve driven. The nervous system provides communication throughout the body as well as organization while the immune system provides surveillance and defense. However, it is important to note that the nervous system is more than just the brain. In the case of an abnormality occurring in the body, an example being when you stub your toe, the nervous system fires off so rapidly that it notifies the brain in seconds. The brain and nervous system are now aware that something went wrong in the body and the brain organizes the next actions to launch.Â
Inflammation is never fate, we have the ability to reduce inflammation and reverse many signs and the progression of the disease. By normalizing the immune system, we will normalize inflammation. If we do not, chronic inflammation leads to depression, insomnia, joint pain, and other autoimmune conditions like diabetes and heart disease. By using a musculoskeletal neuro-inflammatory approach, patients have maximized benefits and improved clinical outcomes are shown.Â
Inflammation Part 2
Acute inflammation is seen as swelling, redness, and tenderness. However, the severe silent inflammation is what is causing the true issues. There are specific biomarkers that we use to assess inflammation. Chronic low-grade inflammation can be tracked with CRP or C Reactive Protein along with other biomarkers including cytokines, neurotransmitters, and oxidative stress markers. Inflammation produces free radicals, which is ultimately the connection between the immune and nervous systems. This occurs in a biochemical timeline along these lines: inflammation is present, inflammation increases pro-inflammatory cytokines, these increase our immune neurotransmitters, which stimulate the increase of free radicals, leading to oxidative stress and the overall derailment of our bodys critical pathways.Â
Testing
Neurotransmitters are seen as moving targets. Sometimes as individuals we are happy, other times sad and so on. This being said, there are tests that capture neurotransmitters but they are seen more as “snapshotsâ€. When using serum to collect neurotransmitters you are only collecting the neurotransmitters at that given moment. One test we use to capture the full range of neurotransmitters is a urine test. The urine is collected over hours, allowing us to see the range and fluctuations in your neurotransmitters. A sample of this test from ZRT Laboratory is shown below:Â
Oxidative Stress
Oxidative stress is essentially an imbalance between free radicals and the body’s antioxidant system. Our body has natural defense systems to protect itself from oxidative stress but when the imbalance is too great, we start to see breakdowns in the body’s pathways. Free radicals are a natural occurrence in ATP synthesis and help to defend against infections as well as signal other cellular functions and regulation. However, when an abundance of free radicals take over the system they begin to damage cell structures, specifically DNA, proteins, and lipids. One specific example is damaged tryptophan resulting in reduced serotonin levels, ultimately leading to bouts of depression, IBS, and insomnia. Great oxidative stress markers we look for in patients include DOPAC, 5HIAA, and Taurine. An example of Comprehensive Urine from Doctors Data is shown below:Â
Genetics, Inflammation, and Oxidative StressÂ
When a patient has severe oxidative stress and inflammation, it is critical for them to be tested for SNPs. In fact, 30-50% of Americans have a polymorphism. When a patient has high inflammatory numbers, for instance, if the glutamine is very high and we do a genetic screening we often find the patient is homozygous negative in SOD2. This specific test result indicates the patient has limited ability to deal with free radicals and may benefit from extra antioxidant support.Â
For more information about SOD2 and its role with oxidative stress, please review the article:Â
“Sirt3 Impairment and SOD2 Hyperacetylation in Vascular Oxidative Stress and Hypertensionâ€
Genetics need to be looked at as functional genetics and it should be understood that the body has the ability to overcome deficiencies when controlled by specific environmental factors. A critical component to reducing inflammation and controlling environmental factors comes from the food we eat. By eating local organic foods, our body will see a reduction in inflammation by a reduction of chemicals. From the kitchen to the genes, everything is related.Â
The older I get, the more I realize that my parents telling me to eat my vegetables was for more benefits than just to grow up “big and strongâ€. The research that has been evolving the past decade points heavily to the fact that what we put in our mouths alters who we are tomorrow. Our genes are constantly changing and charging and are being influenced by the inflammation and nutrients we feed them. If we eat chips and pizza our genes will react to the chemicals in the food and alter their expression, leading to increased inflammation. However, if we eat spinach and organic grass-fed meat our body will break down those nutrients completely different, ultimately altering the genetic expression and thriving with rich phytonutrients. To truly be symptom-free and obtain optimal health, it all starts in the kitchen. -Kenna Vaughn, Senior Health CoachÂ
The scope of our information is limited to chiropractic, musculoskeletal, and nervous health issues or functional medicine articles, topics, and discussions. We use functional health protocols to treat injuries or disorders of the musculoskeletal system. Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We also make copies of supporting research studies available to the board and or the public upon request. To further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us at 915-850-0900. Â
References:Â
Dikalova AE, Itani HA, Nazarewicz RR, et al. Sirt3 Impairment and SOD2 Hyperacetylation in Vascular Oxidative Stress and Hypertension. Circ Res. 2017;121(5):564â€574. doi:10.1161/CIRCRESAHA.117.310933
Kellermann, Gottfried. “Inflammation and Oxidative Stress; Major Players in Clinical Conditions.†Functional Medicine Univeristy . 2020, www. Functionalmedicineuniversity .com/members/1038.cfm.
Disclaimers
Professional Scope of Practice *
The information herein on "Functional Neurology: Inflammation, The Nervous System, and Oxidative Stress" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's wellness blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-C) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on dralexjimenez.com, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card






