Spondyloarthritis is a group of inflammatory, immune-mediated diseases that cause chronic low back pain, inflammation, irritating aches, and pains. The conditions mostly affect the spine but can affect joints in the arms, legs, hips, skin, eyes, and intestines. Spondylitis types can significantly affect daily function, physical activity and compromise bone health.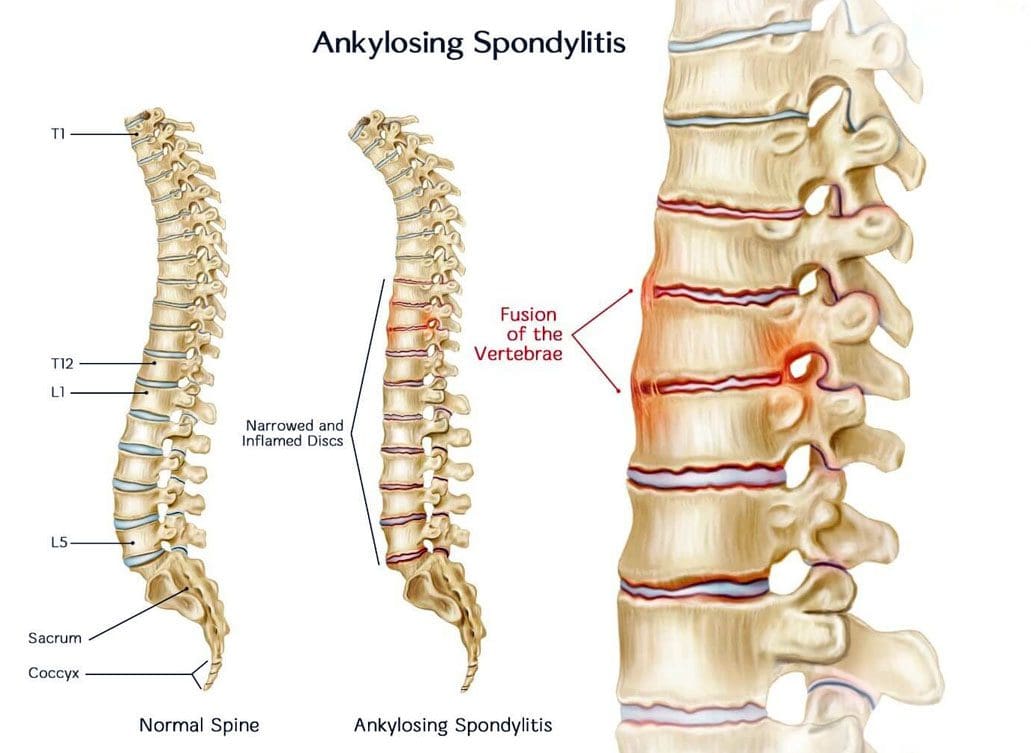
Table of Contents
Spondylitis Types
The main types include:
- Ankylosing spondylitis
- Psoriatic arthritis
- Enteropathic arthritis
- Reactive arthritis
- Juvenile spondylitis
- Undifferentiated spondylitis
Axial Spondylitis vs. Peripheral Spondylitis Types
Spondylitis conditions are classified as axial – axSpA or peripheral – pSpA.
- Axial means relating to the body’s central region, as in the trunk and head.
- Axial spondyloarthritis is arthritis and inflammation in the hips and spine.
- The condition starts before age 45.
- The pain typically starts in the low back but can begin in the neck or other regions.
- Characterized by back pain, usually in the lower back and/or buttocks.
- Morning back stiffness lasting 30 minutes or longer.
- Sacroiliac joint inflammation can also present.
- The back pain gradually progresses.
- Lasts longer than three months.
- Improves with physical movement, not with rest.
- Peripheral spondyloarthritis is arthritis and inflammatory pain in the peripheral joints and tendons and does not include the spine.
- Individuals can have peripheral and axial spondylitis symptoms simultaneously.
- Diagnosis depends on whether symptoms are primarily peripheral or axial.
Spondylitis and Spondylosis
Spondylosis and spondylitis are similar in they cause pain and inflammation in the back and hips. The difference is in each condition’s triggers.
- Spondylitis is a disease in which the body’s immune system degrades joints, causes inflammation, overproduces bone formation, and causes bone fusion.
- Spondylosis is a category of arthritis that presents as the spine ages from normal wear and tear.
- It happens during the degeneration of the spine’s discs and joints.
- It also presents when bone spurs develop on the spine’s vertebrae.
Ankylosing Spondylitis
Ankylosing spondylitis is the most common form of arthritis affecting the spine, other joints, and body regions. The condition causes spinal joint inflammation causing extreme discomfort and chronic pain. In some cases, the inflammation progresses to ankylosis, where spine sections fuse and become immobile. Other body areas that can trigger inflammation include:
- The ribs
- Heels
- Shoulders
- Hips
- Small joints of the feet and hands.
Ankylosing spondylitis symptoms vary from person to person. Common early symptoms include:
- There is general discomfort, appetite loss, and mild fever early in the condition.
- Persistent stiffness and pain in the buttocks and low back, gradually progressing over a couple of weeks or months.
- The pain and stiffness can travel into the neck and spine within months or years.
- The pain is usually spread out and dull.
- The stiffness and pain are worse in the morning and night and improve with light exercise or a warm shower.
- The pain typically becomes chronic, lasts for a minimum of 3 months, and can be felt on both sides.
- Tenderness and pain in the hips, thighs, shoulder blades, heels, and ribs may also occur.
Treatment approaches include applications of ice and heat to reduce swelling, increase circulation, and decrease joint pain, posture exercises, stretches, physical therapy, and medication.
Psoriatic Arthritis
Psoriatic arthritis causes swelling, pain, and inflammation in the small joints of the hands and feet; however, the joints of the knees, ankles, and wrists can also be affected. Psoriasis is a rash that causes scaly skin patches.
- Individuals can develop dactylitis when a finger or toe swells between the surrounding joints.
- Spinal stiffness and pain can present.
- Typically the ends of the finger joints are most affected and experience pain and inflammation.
- The condition also includes fingernail and toenail symptoms.
- Medications frequently utilized to treat ankylosing spondylitis can be used.
- Exercise helps preserve the range of motion and maintain strength.
- Isometric exercises work muscles without joint motion reducing the risk of further injury to inflamed joints.
- Occupational and physical therapy can significantly assist in optimizing arthritic joint function.
Enteropathic Spondylitis
Enteropathic Arthritis is chronic inflammatory arthritis linked to inflammatory bowel disease. The most recognized are Crohn’s and ulcerative colitis.
- The peripheral limb joints and sometimes the whole spine are the most prevalent body areas afflicted with enteropathic spondylitis.
- The main symptom is intestine inflammation, including bowel and joint pain and/or inflammatory back pain.
- Other symptoms can include weight loss, blood in the stool, abdominal pain, and/or chronic diarrhea.
- Managing enteropathic arthritis typically means managing the underlying bowel disease.
Juvenile Spondyloarthritis
Juvenile spondyloarthritis is a group of childhood rheumatic diseases that cause arthritis before age 16 and can continue through adulthood. Juvenile spondyloarthritis encompasses:
- Enteropathic arthritis
- Enthesitis-related arthritis
- Undifferentiated spondyloarthritis
- Psoriatic arthritis
- Reactive arthritis
- Juvenile ankylosing spondylitis
Juvenile spondyloarthritis causes inflammation and pain in joints in the lower body, like the ankles, hips, knees, and pelvis. Other body areas that could be affected include:
- The bowels
- Eyes
- Skin
- Spine
Lethargy and fatigue can also present. The symptoms can be unpredictable and episodic, appearing and disappearing without a specific cause. The condition cycles between flare-ups and remission. Common treatment approaches include:
- Medication
- Exercise
- Posture training
- Physical therapy, medication
- Ice and heat to decrease joint pain and relax muscles.
- In severe cases, surgery could be recommended.
Reactive Arthritis or Reiter’s Syndrome
Reactive arthritis is arthritis that causes pain and inflammation in the mucous membranes, bladder, skin, joints, eyes, and genitals.
- Reactive arthritis is believed to be a reaction to an infection, usually in the gastrointestinal or urinary tract.
- Reactive arthritis does not affect the sacroiliac joints and spine in most cases.
- Reactive arthritis is typically treated with nonsteroidal anti-inflammatory medications, steroids, and rheumatoid arthritis medications.
- A physician could prescribe antibiotics if a bacterial infection brought on reactive arthritis.
Undifferentiated Spondyloarthritis
Undifferentiated spondyloarthritis is where the signs and symptoms of spondylitis don’t meet the criteria for a specific rheumatoid disorder. Individuals diagnosed with undifferentiated spondyloarthritis will have one or more of the symptoms that include:
- Fatigue
- Back inflammation
- Back pain
- Buttock pain that alternates or presents on both sides.
- Swollen toes or fingers
- Heel pain
- Arthritis in the small joints.
- Arthritis in the large limb joints.
- Enthesitis or inflammation where the ligament or tendon connects to the bone.
- Eye inflammation
- Individuals can also present symptoms of other spondylitis types, like psoriatic or ankylosing.
Treatment approaches include:
- Exercise
- Physical therapy
- Posture training
- Ice and heat to decrease joint pain and loosen up muscles.
Spondylitis Types Diagnosis of Spondyloarthritis
References
Carron, Philippe, et al. “Peripheral spondyloarthritis: a neglected entity-state of the art.” RMD open vol. 6,1 (2020): e001136. doi:10.1136/rmdopen-2019-001136
Dougados, Maxime, and Dominique Baeten. “Spondyloarthritis.” Lancet (London, England) vol. 377,9783 (2011): 2127-37. doi:10.1016/S0140-6736(11)60071-8
Gill, Tejpal, et al. “The intestinal microbiome in spondyloarthritis.” Current opinion in rheumatology vol. 27,4 (2015): 319-25. doi:10.1097/BOR.0000000000000187
Rosenbaum, James T. “The eye in spondyloarthritis?.” Seminars in arthritis and rheumatism vol. 49,3S (2019): S29-S31. doi:10.1016/j.semarthrit.2019.09.014
Seo, Mi Ryoung et al. “Delayed diagnosis is linked to worse outcomes and unfavorable treatment responses in patients with axial spondyloarthritis.” Clinical rheumatology vol. 34,8 (2015): 1397-405. doi:10.1007/s10067-014-2768-y
Sharip, Aigul, and Jeannette Kunz. “Understanding the Pathogenesis of Spondyloarthritis.” Biomolecules vol. 10,10 1461. 20 Oct. 2020, doi:10.3390/biom10101461
Disclaimers
Professional Scope of Practice *
The information herein on "Spondylitis Types Injury Medical Chiropractic Health Coach" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's wellness blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-C) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on dralexjimenez.com, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card