
“When a groin strain injury happens, can knowing the symptoms help in the diagnosis, treatment, and recovery times?”
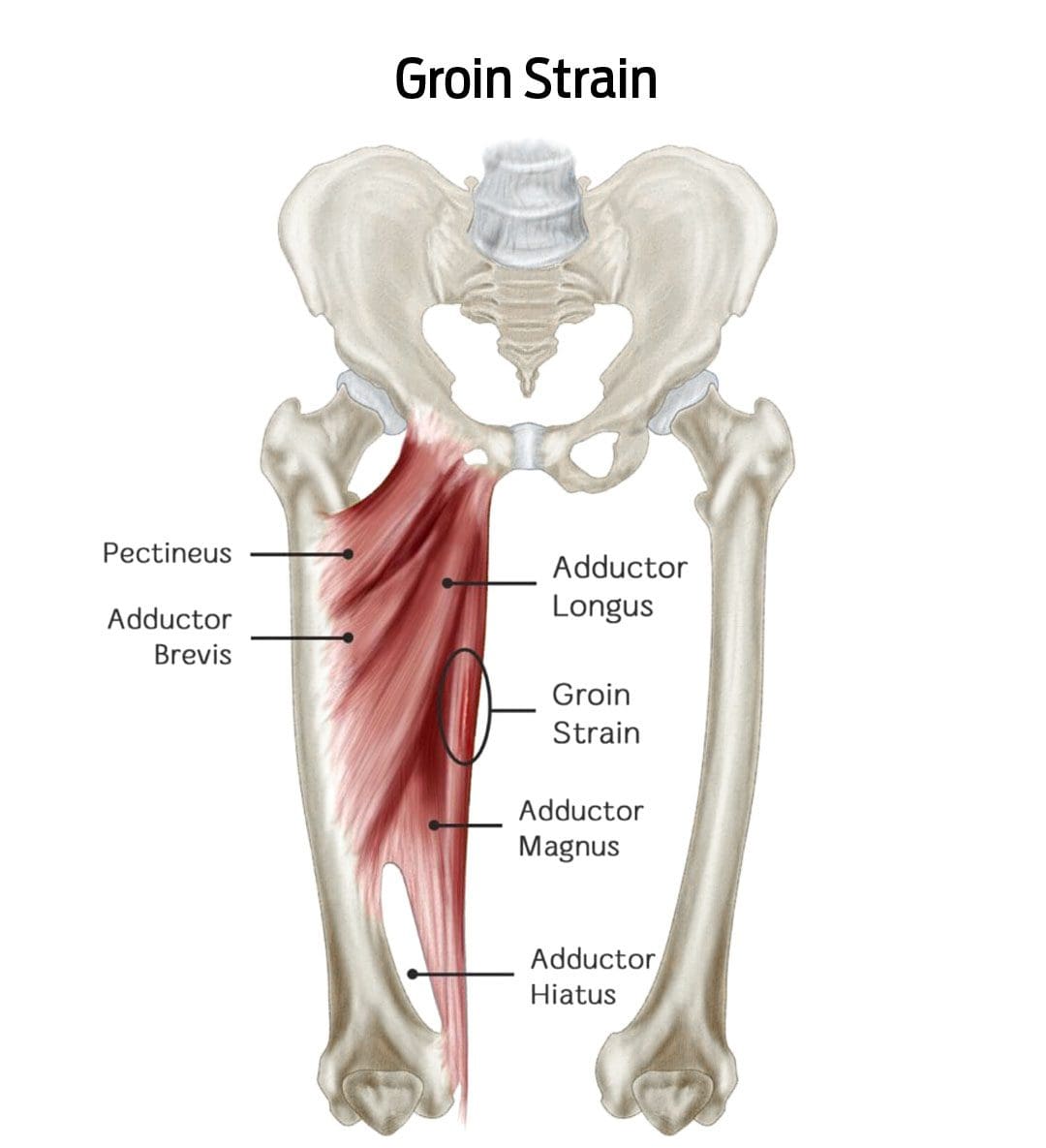
Table of Contents
Groin Strain Injury
A groin strain is an injury to an inner thigh muscle. A groin pull is a type of muscle strain affecting the adductor muscle group (the muscles help pull the legs apart). (Parisa Sedaghati, et al., 2013) The injury is caused when the muscle is stretched beyond its normal range of motion, creating superficial tears. Severe strains can tear the muscle in two. (Parisa Sedaghati, et al., 2013)
- A groin muscle pull causes pain and tenderness that worsens when squeezing the legs together.
- There may also be swelling or bruising in the groin or inner thigh.
- An uncomplicated groin pull takes four to six weeks to heal with proper treatment. (Andreas Serner, et al., 2020)
Symptoms
A groin pull can be painful, interfering with walking, navigating stairs, and/or driving a car. In addition to pain, other symptoms around the injured area include: (Parisa Sedaghati et al., 2013)
- A popping sound or snapping sensation when the injury occurs.
- Increased pain when pulling the legs together.
- Redness
- Swelling
- Bruising of the groin or inner thigh.
Groin pulls are graded by severity and how much they impact mobility:
Grade 1
- Mild discomfort but not enough to limit activities.
Grade 2
- Moderate discomfort with swelling or bruising that limits running and/or jumping.
Grade 3
- Severe injury with significant swelling and bruising can cause pain while walking and muscle spasms.
Signs of a severe groin strain
- Difficulty walking
- Groin pain while sitting or resting
- Groin pain at night
- A healthcare provider should see severe groin pulls because the muscle may have ruptured or be on the verge of rupturing.
- In severe cases, surgery is necessary to reattach the torn ends.
Groin pulls are sometimes accompanied by a stress fracture of the pubis/forward-facing pelvic bones, which can significantly extend healing and recovery time. (Parisa Sedaghati et al., 2013)
Causes
Groin pulls are often experienced by athletes and individuals who play sports where they must stop and change directions quickly, placing excessive strain on the adductor muscles. (Parisa Sedaghati et al., 2013) The risk is increased in individuals who: (T. Sean Lynch et al., 2017)
- Have weak hip abductor muscles.
- Are not in adequate physical condition.
- Have a previous groin or hip injury.
- Pulls can also occur from falls or extreme activities without the proper conditioning.
Diagnosis
A healthcare provider will perform a thorough investigation to confirm the diagnosis and characterize the severity. This involves: (Juan C. Suarez et al., 2013)
Medical History Review
- This includes any previous injuries and specifics about where and when the symptoms started.
Physical Examination
- This involves palpating – lightly touching and pressing the groin region and manipulating the leg to understand better where and how extensive the injury is.
Imaging Studies
- Ultrasound or X-rays.
- If a muscle rupture or fracture is suspected, an MRI scan may be ordered to visualize soft tissue injuries and stress fractures better.
Differential Diagnosis
Certain conditions can mimic a groin pull and require different treatments. These include: (Juan C. Suarez, et al., 2013)
Sports Hernia
- This type of inguinal hernia occurs with sports and work injuries.
- It causes a portion of the intestine to pop through a weakened muscle in the groin.
Hip Labral Tear
- This is a tear in the cartilage ring of the labrum outside the rim of the hip joint socket.
Hip Osteoarthritis
- This is the wear-and-tear form of arthritis that can present with groin pain symptoms.
Osteitis Pubis
- This is inflammation of the pubic joint and surrounding structures, usually caused by the overuse of the hip and leg muscles.
Referred Groin Pain
- This nerve pain originates in the lower back, often due to a pinched nerve, but is felt in the groin.
Treatment
Beginning treatment is conservative and includes rest, ice application, physical therapy, and prescribed gentle stretching and exercises.
- Individuals may need crutches or a walking device to reduce pain and prevent further injury if the pain is significant. (Andreas Serner, et al., 2020)
- Physical therapy will be a part of the treatment plan.
- Over-the-counter pain medications like Tylenol/acetaminophen or Advil/ibuprofen can help with pain relief short term.
- If there is severe pain from a grade 3 injury, prescription medications may be used for a short period to help minimize pain. (Andreas Serner, et al., 2020)
- Surgery is not usually necessary. (Andreas Serner, et al., 2020)
Recovery
Recovery times can vary based on the injury’s severity and physical condition before the injury.
- Most injuries will heal within four to six weeks with rest and proper treatment.
- Severe groin strains can take up to 12 weeks or longer if surgery is involved. (Andreas Serner, et al., 2020)
Injury Rehabilitation
References
Sedaghati, P., Alizadeh, M. H., Shirzad, E., & Ardjmand, A. (2013). Review of sport-induced groin injuries. Trauma monthly, 18(3), 107–112. doi.org/10.5812/traumamon.12666
Serner, A., Weir, A., Tol, J. L., Thorborg, K., Lanzinger, S., Otten, R., & Hölmich, P. (2020). Return to Sport After Criteria-Based Rehabilitation of Acute Adductor Injuries in Male Athletes: A Prospective Cohort Study. Orthopaedic journal of sports medicine, 8(1), 2325967119897247. doi.org/10.1177/2325967119897247
Lynch, T. S., Bedi, A., & Larson, C. M. (2017). Athletic Hip Injuries. The Journal of the American Academy of Orthopaedic Surgeons, 25(4), 269–279. doi.org/10.5435/JAAOS-D-16-00171
Suarez, J. C., Ely, E. E., Mutnal, A. B., Figueroa, N. M., Klika, A. K., Patel, P. D., & Barsoum, W. K. (2013). Comprehensive approach to the evaluation of groin pain. The Journal of the American Academy of Orthopaedic Surgeons, 21(9), 558–570. doi.org/10.5435/JAAOS-21-09-558
Disclaimers
Professional Scope of Practice *
The information herein on "Recognizing Groin Strains: Symptoms & Recovery Time" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's wellness blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-C) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on dralexjimenez.com, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card






