Table of Contents
Traumatic Brain Injury and Posture: How Concussions and Severe TBIs Disrupt Balance—and How Integrative Chiropractic Care Can Help

Key Takeaways
-
TBIs can change posture. Mild TBIs (concussions) can cause long-lasting balance problems by disrupting vision, the vestibular system (inner ear), and body-sense (proprioception). Severe TBIs can cause rigid, reflex body positions called decorticate or decerebrate posturing—a medical emergency. (Cleveland Clinic, 2023; Mount Sinai, n.d.; Sosnoff et al., 2011). PMC+3Cleveland Clinic+3Cleveland Clinic+3
-
Neck alignment matters. Concussions often involve the cervical and upper-thoracic spine. Misalignment here can exacerbate headaches, dizziness, and impaired eye-head coordination, making balance more challenging. (Brain Injury Canada; BIAA; Row et al., 2019). braininjurycanada.ca+2Brain Injury Association of America+2
-
Integrative chiropractic care can be an integral part of recovery, including targeted spinal adjustments, vestibular and ocular motor rehabilitation, and sensory-motor training under the supervision of a nurse practitioner. Early, team-based screening and referral are essential. Evidence for vestibular rehab is stronger than for some other approaches. (AAPMR 2025; Row 2019; Alsalaheen 2013; Mucha/VOMS materials). PMC+3PM&R KnowledgeNow+3PMC+3
-
Severe “abnormal posturing” (decorticate/decerebrate) = call emergency services now. Mount Sinai Health System+1
What Changes After a TBI? Posture, Balance, and the “Balance Triad”
To stand, walk, and turn your head smoothly, your brain blends input from three systems sometimes called the balance triad:
-
Vision: What your eyes see
-
Vestibular system: Inner ear balance organs
-
Somatosensory/proprioception: Body-sense from muscles and joints
A concussion can disturb one or more of these systems, so the brain’s “blending” process becomes less reliable. People may feel unsteady or dizzy in busy environments or wobbly on soft surfaces. Studies show that even with a history of mild TBI, people can have different postural control patterns long after the early symptoms fade (Sosnoff et al., 2011). (Row 2019 also highlights objective balance tools that pick up these changes.) (Sosnoff et al., 2011; Row et al., 2019; AAPMR, 2025; Brain Injury Canada). braininjurycanada.ca+3PMC+3PMC+3
Typical day-to-day signs after a concussion
-
Feeling “off-balance” when turning quickly or walking in a grocery store aisle
-
Headaches, neck pain, eye strain, motion sensitivity
-
Trouble with tandem walking (heel-to-toe) or maintaining balance with eyes closed
-
Symptoms that flare with neck movement or screen time (PCS/PSaC literature) (Permenter et al., 2023; Broshek et al., 2022). NCBI+1
When Posture Becomes an Emergency: Decorticate and Decerebrate Posturing
In severe TBIs, the body can assume rigid, reflexive positions:
-
Decorticate posturing: arms flexed and pulled to the chest; legs straight and rigid
-
Decerebrate posturing: arms and legs extended straight; head/neck arched back; toes pointed
Both postures signal serious brain damage and require immediate emergency care. Do not wait; call emergency services. (Cleveland Clinic; Mount Sinai). Cleveland Clinic+1
Clinically, these postures are assessed in conjunction with other neurological findings (e.g., Glasgow Coma Scale) to guide urgent care, airway management, and transfer to a neurotrauma center. (Cleveland Clinic; StatPearls DAI). Cleveland Clinic+1
The Neck–Brain Connection: Why Cervical and Upper-Thoracic Alignment Matters
After a TBI—especially one involving whiplash—the cervical (neck) and upper thoracic spine often become stiff, tender, or misaligned. This can alter:
-
Head position (affecting eye-head reflexes)
-
Proprioceptive input from neck joints and muscles
-
Vestibular integration (neck and inner ear signals must agree)
When neck mechanics are poor, headaches, dizziness, and blurred or unstable vision can worsen, which makes balance harder. This is why many concussion plans include a cervical exam and treatment for neck-driven symptoms along with vestibular/oculomotor work. (Brain Injury Canada; BIAA; Row 2019; AAPMR). PM&R KnowledgeNow+3braininjurycanada.ca+3Brain Injury Association of America+3
How Integrative Chiropractic Care Can Support Recovery
Important: Chiropractic care does not replace medical care for TBIs. It can be a complement within a coordinated plan supervised by a licensed medical professional (e.g., nurse practitioner). The strongest research support is found for vestibular and oculomotor rehabilitation, as well as for objective balance assessment. Evidence for other mechanisms (e.g., enhancing blood or cerebrospinal fluid flow via manual techniques) is more preliminary; use cautious, individualized application. (Row 2019; Alsalaheen 2013; AAPMR 2025; Impact Medical Group explainer). Impact Medical Group+3PMC+3d-scholarship.pitt.edu+3
1) Spinal adjustments for alignment and mobility
Gentle, targeted adjustments may reduce neck stiffness, improve segmental motion, and normalize some proprioceptive input from the cervical and upper thoracic spine, potentially easing headaches and dizziness associated with neck dysfunction. (Northwest Florida Physicians Group; Vida Integrated Health explainer). Northwest Florida Physicians Group+1
2) Vestibular and oculomotor rehab
Exercises that retrain gaze stability, saccades, visual motion tolerance, and head-eye coordination (e.g., VOMS-guided programming) have growing evidence in concussion care. (VOMS materials; Elbin et al., 2018; AAPMR, 2025). PMC+2health.mil+2
3) Sensory-motor training
Balance drills that challenge vision, somatosensation, and vestibular input (e.g., compliant surfaces, narrow stance, head turns) help the brain “re-blend” signals. Objective platforms, such as the Sensory Organization Test (SOT), quantify progress. (Row 2019; SOT RehabMeasures). PMC+1
4) Team-based care and symptom management
Care often includes sleep, stress management, and pacing strategies, as well as hydration/nutrition support, and stepwise return-to-life plans. (Pinnacle Health Chiro blog; systematic reviews on persistent symptoms). pinnaclehealthchiro.com+1
Clinical perspective—Dr. Alexander Jimenez, DC, APRN, FNP-BC:
In our integrative clinic, we screen for cervico-vestibular contributors to dizziness and headaches after concussion. Under nurse-practitioner supervision, we combine gentle spinal work for neck mechanics with vestibular/oculomotor drills, breathing and posture retraining, and objective balance measures to guide progression. Patients are referred promptly for neuroimaging or specialty care when red flags appear. El Paso, TX Doctor Of Chiropractic
Tests and Tools—From Simple to Advanced
Below is a practical, simple-to-advanced list you can expect your care team to use. The goal is safety first, followed by quick screening, then targeted and objective testing.
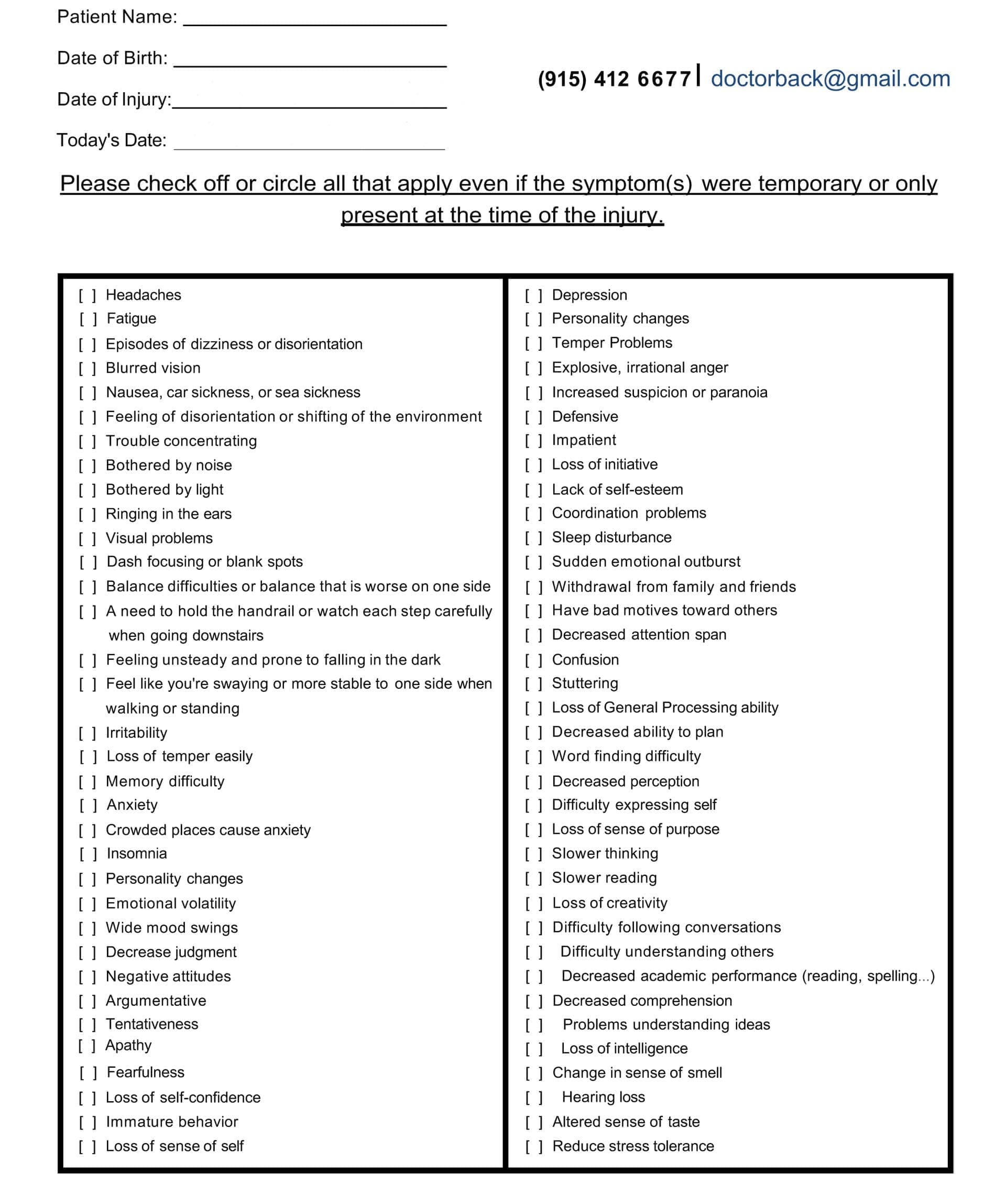
Symptom Questionnaire:
A. Initial Screening (Sideline/Clinic Basics)
-
Symptom scales & history interview (headache, dizziness, sleep, mood). (StatPearls PCS). NCBI
-
Neurologic screen & red-flags check (worsening headache, vomiting, severe neck pain/limited ROM, focal deficits). Emergency posturing = 911. (Mount Sinai; Cleveland Clinic). Mount Sinai Health System+1
-
Cervical exam (ROM, tenderness, joint and muscle dysfunction). (AAPMR; Row 2019). PM&R KnowledgeNow+1
B. Bedside Balance & Posture Checks
-
Romberg / tandem stance and gait (eyes open/closed).
-
BESS (Balance Error Scoring System): quick clinic test with documented utility in concussion populations. (Bell et al., 2011; APTA; RehabMeasures). PMC+2apta.org+2
-
mCTSIB / foam stance to stress proprioceptive vs. visual input (often integrated with BESS/SOT workflows). (Row 2019). PMC
C. Vestibular & Oculomotor Screens
-
VOMS (Vestibular/Ocular Motor Screening): quick provocation screen for smooth pursuit, saccades, VOR, convergence, and visual motion sensitivity. (Mucha et al.; Military Health VOMS; Elbin et al., 2018). PMC+1
-
Near-point convergence and head-impulse style bedside checks to flag referral needs (often embedded in VOMS). (VOMS resources). ImPACT Applications
D. Objective Balance and Vestibular Testing
-
SOT (Sensory Organization Test) posturography: widely cited for quantifying use of visual, vestibular, and proprioceptive inputs. (Row 2019; RehabMeasures SOT). PMC+1
-
Head-Shake SOT variants to assess balance while the head moves (useful when routine SOT is normal). (Heick 2023; Roberts 2024). International Journal of Sports Therapy+1
-
Instrumented BESS (force plates/wearables) for detailed sway metrics when available. (Schönberg 2024). MDPI
E. Targeted Vestibular Diagnostics
-
Dix-Hallpike for BPPV (positional vertigo) when symptoms are positional.
-
Specialty vestibular testing as needed (video head impulse, calorics, VNG), guided by physiatry/ENT/neurology. (AAPMR 2025). PM&R KnowledgeNow
F. Neurocognitive / Multidomain Tools
-
Neurocognitive testing (utilizing clinic-based platforms) is used in conjunction with, not instead of, clinical judgment.
-
Psychological screening when chronic pain, anxiety, or depression complicate recovery, since these factors can mimic or magnify “post-concussive” symptoms. (Iverson 1997; Snell 2018; Rosenbloom 2013). PubMed+2PubMed+2
G. Imaging (When Indicated)
-
CT head for acute red flags (rule out bleeding/fracture).
-
MRI (including DTI) if persistent deficits or suspected diffuse axonal injury—ordered by the medical team. (StatPearls DAI). NCBI
Why Balance Problems Persist
-
Some people develop persistent symptoms after concussion (PSaC) even after the typical 2-week recovery window. These can include dizziness, sleep disturbances, headaches, cognitive impairment, and mood changes. (StatPearls PCS; Quinn 2018; Broshek 2022). NCBI+2PMC+2
-
Vestibular problems are common during recovery and can affect work and quality of life. (Marcus 2019; AAPMR 2025). PMC+1
-
Chronic pain and psychological stressors can overlap with, or imitate, post-concussive symptoms—so plans should address both biologic and psychosocial needs. (Iverson 1997; Snell 2018; Rosenbloom 2013). PubMed+2PubMed+2
A Practical, Step-by-Step Integrated Care Plan
Always involve a licensed medical professional for screening, imaging decisions, and medication management. Severe symptoms or abnormal posturing = emergency care.
Step 1 — Medical Screen & Safety
-
Rule out red flags (worsening headache, severe neck pain, repeated vomiting, new weakness/numbness, abnormal posturing). (Cleveland Clinic; Mount Sinai). Cleveland Clinic+1
Step 2 — Baseline Measures
-
Document symptoms, sleep, exercise tolerance, and triggers.
-
Bedside balance tests (BESS, tandem gait), VOMS, and cervical exam. (Bell 2011; VOMS; Row 2019). PMC+2PMC+2
Step 3 — Early Cervico-Vestibular Care
-
Gentle spinal adjustments to improve neck mobility and reduce headache/neck-driven dizziness in appropriate patients.
-
Vestibular/oculomotor drills (gaze stability, saccades, convergence) progressed gradually. (Vida; Northwest Florida Physicians Group; VOMS). Vida Integrated Health+2Northwest Florida Physicians Group+2
Step 4 — Objective Balance Training
-
Integrate SOT-guided balance work and head-movement balance when tolerated. (Row 2019; Heick 2023). PMC+1
Step 5 — Whole-Person Support
-
Sleep hygiene, stress management, graded activity, and nutrition/hydration. These can influence recovery and pain. (Pinnacle Health; Rosenbloom 2013). pinnaclehealthchiro.com+1
Step 6 — Re-evaluate and Escalate
-
If dizziness, imbalance, or cognitive issues persist, the NP or MD may order an MRI/DTI or refer the patient to neurology, physiatry, or ENT. (StatPearls DAI; AAPMR). NCBI+1
Dr. Jimenez’s clinic approach: Patients with concussion-related dizziness often show subtle cervical dysfunction plus vestibular/oculomotor intolerance. We blend neck-focused manual care with VOMS-informed exercise progressions, update objective balance metrics, and communicate closely with the medical team for imaging or pharmacologic needs. El Paso, TX Doctor Of Chiropractic
What About Blood Flow or CSF Flow?
Some chiropractic sources propose that restoring spinal alignment may support blood flow or cerebrospinal fluid (CSF) dynamics. The biological idea is plausible, but direct clinical evidence in concussion patients is limited; use cautious, individualized care and prioritize evidence-supported elements like vestibular rehab and objective testing. (Impact Medical Group explainer; HML Functional Care overview). Impact Medical Group+1
When to Seek Emergency Care—Right Now
-
Abnormal posturing (decorticate/decerebrate), confusion that worsens, seizure, severe or increasing headache, repeated vomiting, weakness/numbness, slurred speech, loss of consciousness, or suspected skull/neck fracture. (Cleveland Clinic; Mount Sinai; StatPearls). Cleveland Clinic+2Mount Sinai Health System+2
Frequently Asked Questions
Is it normal to feel “off” for weeks?
Many improve in 2–4 weeks, but a significant minority have persisting symptoms. Targeted rehab and team-based care help. (Quinn 2018; Broshek 2022). PMC+1
Can vestibular rehab help even months later?
Yes. Evidence supports vestibular/oculomotor rehab for ongoing dizziness and balance issues after TBI. (Alsalaheen 2013; AAPMR 2025; Row 2019). d-scholarship.pitt.edu+2PM&R KnowledgeNow+2
Do I need imaging?
Imaging is ordered by the medical team based on red flags and exam; many concussions do not need CT or MRI initially. Persistent or severe deficits may prompt MRI/DTI. (StatPearls DAI). NCBI
Final Word
-
Mild TBI can quietly shift how your brain controls posture—and those changes can last unless you retrain the system.
-
Severe TBI with abnormal posturing is an emergency.
-
An integrated plan—comprising medical oversight, cervical care, vestibular/oculomotor rehabilitation, and objective balance tracking—provides a practical path back to confident movement.
References
-
Decorticate Posturing: What It Is, Causes, & Treatment. Cleveland Clinic. Last reviewed May 9, 2023. Cleveland Clinic
-
Decerebrate Posturing: What It Is, Causes, & Treatment. Cleveland Clinic. Last reviewed May 9, 2023. Cleveland Clinic
-
Decorticate posture Information. Mount Sinai Health Library. Mount Sinai Health System
-
Decerebrate posture Information. Mount Sinai Health Library. Mount Sinai Health System
-
Previous Mild Traumatic Brain Injury and Postural-Control Dynamics. (Sosnoff et al., 2011). PMC
-
Mobility After Brain Injury (Balance Overview). Brain Injury Canada. braininjurycanada.ca
-
Factors Associated with Sitting and Standing Balance (TBI Model Systems). Brain Injury Association of America. Brain Injury Association of America
-
Posturing After Brain Injury Explained: Decerebrate vs Decorticate. Flint Rehab. Flint Rehab
-
Using Chiropractic Care to Treat Traumatic Brain Injuries. Northwest Florida Physicians Group. Northwest Florida Physicians Group
-
Can Chiropractic Care Help With Mild Traumatic Brain Injuries? Impact Medical Group (2024). Impact Medical Group
-
Treating Concussions with Chiropractic Care. Vida Integrated Health. Vida Integrated Health
-
How Chiropractic Neurology Supports Brain Healing. HML Functional Care. HML Functional Care
-
Six Ways Chiropractic Care Supports Healing After TBI. Pinnacle Health Chiropractic. pinnaclehealthchiro.com
-
Balance Assessment in Traumatic Brain Injury. (Row et al., 2019). PMC
-
Vestibular Dysfunction (after brain injury). AAPMR KnowledgeNow (updated Jan 9, 2025). PM&R KnowledgeNow
-
A Brief Vestibular/Ocular Motor Screening (VOMS) Assessment to Evaluate Concussions: Preliminary Findings. (Elbin et al., 2018) & VOMS Instructions/Scorecards. PMC+1
-
Systematic Review of the Balance Error Scoring System (BESS). (Bell et al., 2011); BESS (APTA; RehabMeasures). PMC+2apta.org+2
-
Sensory Organization Test (RehabMeasures). Shirley Ryan AbilityLab
-
Head-Shake SOT (Heick et al., 2023) and HS-SOT Norms (Roberts et al., 2024). International Journal of Sports Therapy+1
-
Postconcussive Syndrome. StatPearls (Permenter et al., 2023). NCBI
-
Prolonged Postconcussive Symptoms. (Quinn et al., 2018). PMC
-
Persisting Symptoms after Concussion (PSaC): Time for a Paradigm Shift. (Broshek et al., 2022). PMC
-
Vestibular dysfunction in acute traumatic brain injury. (Marcus et al., 2019). PMC
-
‘Postconcussive’ symptoms in persons with chronic pain. (Iverson et al., 1997). PubMed
-
Untangling chronic pain and post-concussion symptoms. (Snell et al., 2018). PubMed
-
Diffuse Axonal Injury. StatPearls (Mesfin et al., 2023). NCBI
-
Dr. Alexander Jimenez, DC, APRN, FNP-BC (clinic and professional profile). El Paso, TX Doctor Of Chiropractic
Disclaimers
Professional Scope of Practice *
The information herein on "Traumatic Brain Injury and Posture: Treatment Options" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's wellness blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-C) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on dralexjimenez.com, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card