“Can spinal stenosis physical therapy improve quality of life and decrease pain symptoms for individuals dealing with the degenerative condition?”
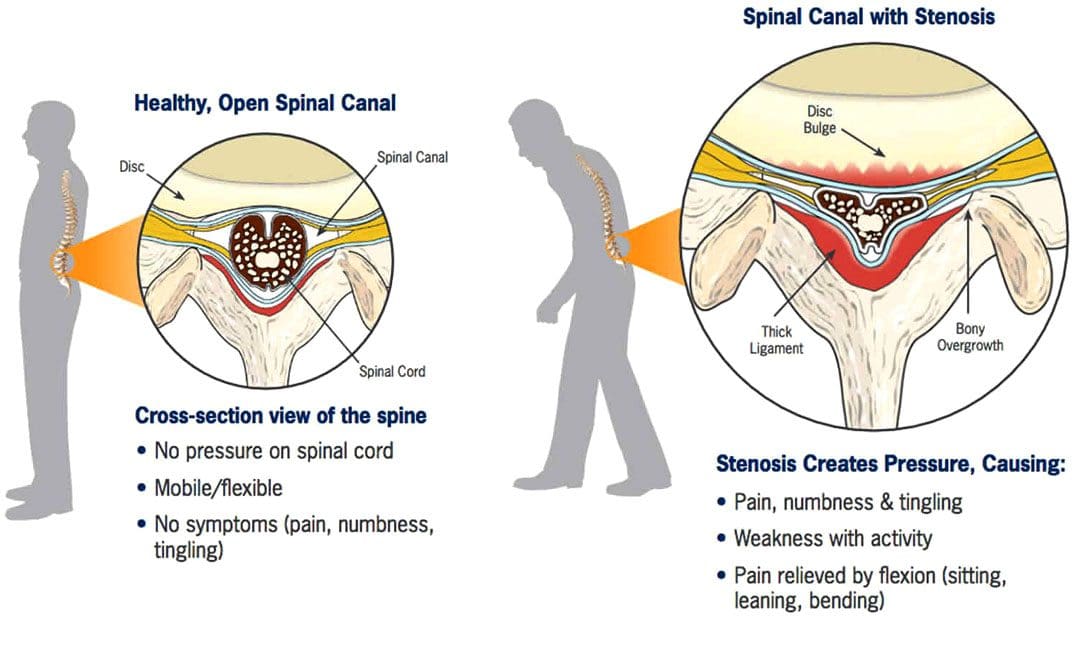
Table of Contents
Spinal Stenosis Physical Therapy
Spinal stenosis causes narrowing of the openings of the vertebrae. The affected openings are either:
- The central spinal canal – where the spinal cord sits.
- Foramen – the small openings on the sides of each vertebra where nerve roots branch off from the spinal cord.
- Spinal stenosis is most common in the lumbar spine/lower back.
- It can also occur in the cervical spine/neck. (Jon Lurie, Christy Tomkins-Lane 2016)
The discs between the spine’s vertebrae provide cushioning and shock absorption in the spine and the rest of the body. Degenerative changes to the discs are believed to be the start of spinal stenosis. When the discs lack sufficient hydration/water and disc height decreases over time, the cushioning and shock absorption becomes less and less effective. The vertebrae can then become compressed, causing friction. Degenerative spinal stenosis can also develop from excess scar tissue and bone spurs (growth that develops on the edge of a bone) that can form after injury or spinal surgery.
Assessment
A physician will make a diagnosis of spinal stenosis. The doctor will take an imaging scan of the spine to determine the exact location of the degeneration and to measure how narrow the openings have become. Pain, stiffness, limited mobility, and loss of range of motion are often present. If spinal stenosis has caused nerve compression, there may also be pain, numbness, tingling, or weakness in the buttocks (sciatica), thighs, and lower legs. A physical therapist will determine the degree by assessing the following:
- Vertebrae mobility – how the spine bends and twists in different directions.
- Ability to change positions.
- The strength of the core, back, and hip muscles.
- Balance
- Posture
- Gait pattern
- Nerve compression to determine if there are any symptoms in the legs.
- Milder cases usually do not involve nerve compression, as back stiffness is more common.
- In more severe cases, there may be significant pain, limited mobility, and nerve compression, causing leg weakness.
The most common symptom of spinal stenosis is increased pain with backward bending or extension of the lumbar spine. This includes positions that extend the spine, such as standing, walking, and lying on the stomach. Symptoms usually improve when bending forward and when the spine is positioned more into a flexed or bent position, like when sitting and reclining. These body positions open up the spaces in the central spinal canal.
Surgery
Spinal stenosis is the most common reason for undergoing surgery in adults 65 and older. However, surgery is almost always performed as a last resort if pain, symptoms, and disability persist after trying conservative therapies, including chiropractic, non-surgical decompression, and physical therapy, for months or years. The severity of symptoms and current state of health will determine whether a doctor will recommend surgery. (Zhuomao Mo, et al., 2018). Conservative measures can be safer and just as effective. A systematic review or study based on all available primary research found that physical therapy and exercise resulted in similar outcomes to surgery for improving pain and disability. (Zhuomao Mo, et al., 2018). Except for severe cases, surgery is often not necessary.
Physical Therapy for Spinal Stenosis
The objective of physical therapy includes:
- Decreasing pain and joint stiffness.
- Relieving nerve compression.
- Reducing tightness in the surrounding muscles.
- Improving the range of motion.
- Improving postural alignment.
- Strengthening the core muscles.
- Improving leg strength to help with balance and overall function.
- Stretching of the back muscles, including those running vertically along the spine and those running diagonally from the pelvis to the lumbar spine, helps relieve muscle tightness and pain and can improve overall mobility and range of motion of the lumbar spine.
- Stretching the hip muscles, including the hip flexors in the front, the piriformis in the back, and the hamstrings that run from the back of the hip down the leg to the knee, is also important as these muscles are attached to the pelvis, which directly connects to the spine.
- Exercises for strengthening the abdominal core muscles, including the muscles in the trunk, pelvis, lower back, hips, and abdomen, help stabilize the spine and protect it from excessive movement and compressive forces.
- With spinal stenosis, the core muscles often become weak and inactive and unable to do their job to support the spine. Core exercises often begin by activating the deep abdominal muscles while lying flat on the back with the knees bent.
- Exercises will progress as the individual gains more strength and control as the spine stabilizes.
- Spinal stenosis physical therapy will also involve balance training and glute exercises for strengthening the leg muscles.
Prevention
Working with a physical therapist can help prevent future problems by maintaining spinal mobility, keeping the individual active, and exercising to maintain strength and stability to provide a solid foundation to support the lower back and prevent symptoms from worsening.
Severe Spinal Stenosis Physical Therapy
Physical therapy usually involves performing stretches for the lower back, hips, and legs, mobility exercises, and core strengthening exercises to improve spinal support and decrease pain. Treatments like heat or electrical stimulation may also be used on a case-by-case basis if there is significant pain or tightness in the back muscles. However, there is not enough clinical evidence to support that there are additional benefits. (Luciana Gazzi Macedo, et al., 2013) The effectiveness of physical therapy is high because surgery alone cannot strengthen the muscles that stabilize the spine, increase the mobility or flexibility of the surrounding muscles, and improve postural alignment.
The Root Causes of Spinal Stenosis
References
Lurie, J., & Tomkins-Lane, C. (2016). Management of lumbar spinal stenosis. BMJ (Clinical research ed.), 352, h6234. doi.org/10.1136/bmj.h6234
Mo, Z., Zhang, R., Chang, M., & Tang, S. (2018). Exercise therapy versus surgery for lumbar spinal stenosis: A systematic review and meta-analysis. Pakistan journal of medical sciences, 34(4), 879–885. doi.org/10.12669/pjms.344.14349
Macedo, L. G., Hum, A., Kuleba, L., Mo, J., Truong, L., Yeung, M., & Battié, M. C. (2013). Physical therapy interventions for degenerative lumbar spinal stenosis: a systematic review. Physical therapy, 93(12), 1646–1660. doi.org/10.2522/ptj.20120379
Disclaimers
Professional Scope of Practice *
The information herein on "Spinal Stenosis Physical Therapy: Improving Quality of Life" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's wellness blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-C) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on dralexjimenez.com, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card