Table of Contents
The Missed Signs of Traumatic Brain Injury (TBI): How Chiropractors and Nurse Practitioners Find What Others Overlook—and Guide Recovery

Why TBIs get missed more often than you think
Many people with a traumatic brain injury “look fine,” especially after a mild concussion. Symptoms can be subtle, delayed, and easy to misread as stress, poor sleep, or mood issues. These hidden problems often appear days or weeks after the injury, which is one reason front-line providers or urgent care teams may not catch them at first. (BrainLine, 2018). BrainLine
Legal and clinical consumer guides make the same point: even in emergency settings, TBI signs are often overlooked, and family members are sometimes the first to notice behavioral changes such as irritability, slowed thinking, or problems with taste and smell. (Fisher Stark, 2021). Fisher Stark P.A.
Military health experts call these “invisible wounds.” They stress that recognizing symptoms early—headache, sleep problems, balance issues, slowed thinking, word-finding trouble, irritability, and mood swings—helps recovery and prevents setbacks. (U.S. Air Force, 2017). Hanscom Air Force Base
What “hidden symptoms” look like in real life
Hidden TBI symptoms often affect thinking, emotions, and the senses. Patients may experience:
-
Cognitive: trouble concentrating, slowed reading or speaking, memory slips, mental fatigue. (BrainLine, 2018). BrainLine
-
Emotional/Behavioral: irritability, mood swings, anxiety, or depression that the patient may not recognize—but loved ones do. (Fisher Stark, 2021; U.S. Air Force, 2017). Fisher Stark P.A.+1
-
Sensory: changes in smell or taste, ringing in the ears, light or sound sensitivity, visual blurring, or “tired eyes.” (BrainLine, 2018; Fisher Stark, 2021). BrainLine+1
-
Physical: headache, dizziness, nausea, fatigue, sleep changes, unsteady balance, or coordination problems. (Mayo Clinic, n.d.; BrainLine, 2018). Mayo Clinic+1
Key idea: These symptoms can start late or fluctuate. Without a thorough interview and repeat check-ins, they’re easy to miss. (BrainLine, 2018). BrainLine
How a chiropractor or nurse practitioner uncovers what others miss
Step 1: A comprehensive history—lots of questions on purpose
A careful clinician starts with a timeline (how/when the injury happened), red flags (worsening headache, repeated vomiting, confusion), and a symptom map that covers thinking, mood, sleep, balance, neck pain, and the senses. Typical questions include:
-
Mechanism & prior injuries: How fast? Any whiplash? Previous concussions?
-
Cognition & school/work: Do tasks take longer? Do you lose your place while reading?
-
Emotion & behavior: Are you more irritable or anxious than usual?
-
Sleep: Trouble falling or staying asleep? Sleeping too much?
-
Sensory changes: Any change in smell/taste? Light or sound sensitivity?
-
Headache & neck: Location, triggers (screens, noise), neck stiffness?
-
Balance & vision: Feeling “off-balance,” drifting when walking, blurred vision, or difficulty focusing?
-
Lifestyle & meds: Hydration, caffeine, alcohol, new medications, or supplements?
-
Work/sport demands: Screen time, loud settings, driving, sport return plans?
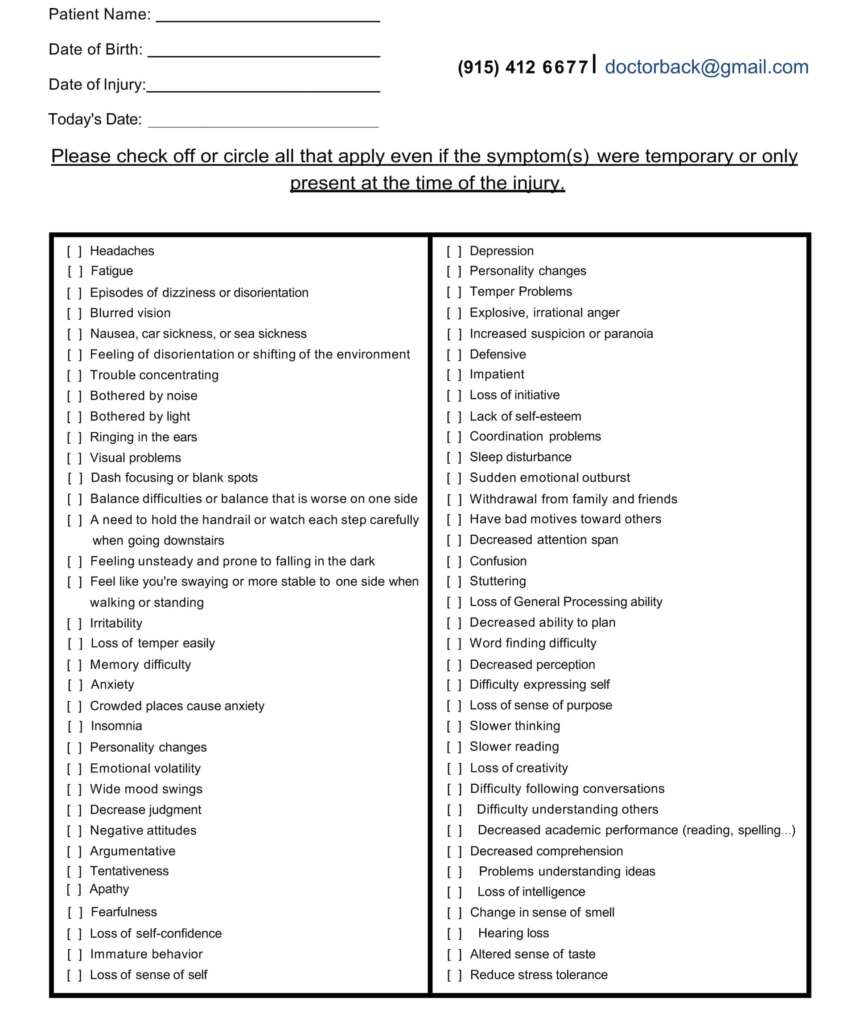
This questioning targets the subtle signs documented by brain injury resources and health systems. (BrainLine, 2018; Mayo Clinic, n.d.; U.S. Air Force, 2017; Fisher Stark, 2021). Fisher Stark P.A.+3BrainLine+3Mayo Clinic+3
Step 2: Focused exams that connect the dots
Beyond standard neurological checks (alertness, pupils, strength, sensation), clinicians add:
-
Cervicogenic screening: neck joint and soft-tissue assessment (often relevant to whiplash). (Denver Chiropractic, n.d.). Denver Integrated Spine Center
-
Balance and gait checks: tandem stance/walk, single-leg stance, and head-turn walk to assess vestibular function. (BrainLine, 2018). BrainLine
-
Eye-movement and vestibular-ocular screening: pursuit, saccades, gaze stabilization, and reports of light/motion sensitivity. (BrainLine, 2018). BrainLine
-
Symptom inventories: simple scales to track headache, dizziness, mental fog, sleep, and mood over time. (BrainLine, 2018; U.S. Air Force, 2017). BrainLine+1
Basic-to-advanced diagnostic tools and assessments
Think of evaluation as a ladder—start with basic tools for everyone, then climb as symptoms or risks become more complex.
Basic tools (everyone with suspected TBI)
-
Detailed history + symptom checklists (as above). (BrainLine, 2018). BrainLine
-
Focused neurological exam (pupils, strength, sensation, reflexes). (Mayo Clinic, n.d.). Mayo Clinic
-
Balance and eye-movement screening for vestibular involvement. (BrainLine, 2018). BrainLine
-
Cervical spine/whiplash assessment because neck issues can drive headaches and dizziness. (Denver Chiropractic, n.d.). Denver Integrated Spine Center
Intermediate tools (when symptoms persist or are complex)
-
Formal cognitive screening (brief paper-and-pencil or tablet-based tests to flag memory, attention, and processing speed). (BrainLine, 2018). BrainLine
-
Targeted vestibular/oculomotor testing if dizziness, visual strain, or motion sensitivity is prominent. (BrainLine, 2018). BrainLine
-
Medical imaging when indicated:
-
CT for suspected bleeding or severe head injury/red flags.
-
MRI for persistent or unexplained symptoms beyond the acute phase. (Mayo Clinic, n.d.). Mayo Clinic
-
-
Headache classification and medication review to reduce rebound or side effects. (Mayo Clinic, n.d.). Mayo Clinic
Advanced or specialist tools (selected cases)
-
Neuropsychological testing for detailed cognitive profiling when return-to-work or complex learning demands are in play. (BrainLine, 2018). BrainLine
-
Multidisciplinary rehabilitation planning (e.g., adding chiropractic care to a rehab team) to address neck dysfunction, headaches, and balance problems. (Chiropractic & Manual Therapies, 2018). BioMed Central
-
Specialty nursing protocols to prevent secondary injury in hospitalized or higher-risk patients—continuous neuromonitoring, metabolic tracking, and family education. (Figueiredo et al., 2024). MDPI
Bottom line: Start simple and escalate as needed. A thorough initial screen plus tiered testing catches most hidden problems while avoiding unnecessary imaging. (Mayo Clinic, n.d.; BrainLine, 2018). Mayo Clinic+1
The integrative model: chiropractor + nurse practitioner
A team approach covers both the neuromusculoskeletal side (neck, balance, proprioception) and the medical side (sleep, mood, medications, and systemic health). Multidisciplinary teams that include chiropractic professionals are commonly used to support TBI-related neck pain, dizziness, headaches, and balance challenges. (Chiropractic & Manual Therapies, 2018; NWHSU, n.d.). BioMed Central+1
What the chiropractor addresses
-
Spinal adjustments (applied judiciously), joint mobilization, and soft-tissue therapy to reduce cervicogenic headache drivers and improve neck mechanics that can aggravate dizziness or visual strain. (Denver Chiropractic, n.d.). Denver Integrated Spine Center
-
Gentle vestibular and proprioceptive drills to retrain balance and gaze stability when appropriate as part of an active care plan. (BrainLine, 2018). BrainLine
-
Exercise-based rehabilitation for posture, eye-head coordination, and upper-cervical control. Some clinics also emphasize circulation and cerebrospinal dynamics as part of a holistic framework. (Pinnacle Health Chiropractic, n.d.). Pinnacle Health Chiropractic
Emerging “chiropractic neurology” programs also highlight non-drug strategies to stimulate targeted neural pathways and support brain function, often blending manual care with sensorimotor training and lifestyle coaching. (HML Functional Care, n.d.). HML Functional Care
What the nurse practitioner covers
-
Medical supervision: ruling out emergencies, setting imaging thresholds (CT/MRI), medication review, and coordinating referrals for neuropsychology or neurology. (Mayo Clinic, n.d.). Mayo Clinic
-
Prevention of “secondary injury” risks in higher-acuity settings: monitoring intracranial pressure surrogates, oxygenation, temperature, and hemodynamics; educating family; and training staff. (Figueiredo et al., 2024). MDPI
-
Whole-person support: sleep hygiene, pacing strategies, return-to-learn/work, stress reduction, and nutrition guidance. (U.S. Air Force, 2017). Hanscom Air Force Base
Why this partnership works
TBI rarely affects only one system. Pairing musculoskeletal expertise with medical oversight helps address the neck-brain connection, medication side effects, sleep and mood problems, and graded return to activity—together. (Chiropractic & Manual Therapies, 2018; NWHSU, n.d.). BioMed Central+1
Dr. Alexander Jimenez’s clinical perspective
In integrative clinics like Dr. Alexander Jimenez’s practice in El Paso, care blends chiropractic methods with medical and functional evaluations (diagnostics, imaging pathways, and lifestyle coaching). His platform emphasizes multi-modal assessment, head/neck injury management, and coordinated return-to-work/sport planning under a dual-scope model (DC + APRN). (Jimenez, n.d.). El Paso, TX Doctor Of Chiropractic
Putting it all together: a practical pathway from first visit to follow-up
1) First visit (Week 0–1)
-
Screen for red flags ? emergency evaluation if present (severe or worsening headache, repeated vomiting, unequal pupils, new weakness, seizure, or altered consciousness). (BrainLine, 2018). BrainLine
-
Deep history + exam with symptom mapping; add balance/vestibular and cervical screening; start a symptom diary. (BrainLine, 2018; Denver Chiropractic, n.d.). BrainLine+1
-
Early plan: relative rest (not bed rest), light activity as tolerated, headache hydration/sleep routines, screen-time limits, and neck pain strategies. (U.S. Air Force, 2017). Hanscom Air Force Base
2) Early follow-up (Week 1–3)
-
Chiropractic care: gentle joint and soft-tissue care, posture work, and beginner eye-head coordination drills. (Pinnacle Health Chiropractic, n.d.). Pinnacle Health Chiropractic
-
NP care: adjust meds if headaches or sleep worsen; consider MRI if symptoms persist or don’t fit the pattern; coordinate formal cognitive screening as needed. (Mayo Clinic, n.d.). Mayo Clinic
-
Education: pacing (“do-tolerate-pause-repeat”), hydration and nutrition, and graded return to work/school with breaks. (U.S. Air Force, 2017). Hanscom Air Force Base
3) Ongoing care (Week 3+)
-
Progression of rehab: more advanced vestibular and balance tasks; functional neck strengthening, and ergonomic coaching for screens/driving. (BrainLine, 2018; Denver Chiropractic, n.d.). BrainLine+1
-
Team huddles: if a plateau occurs, add neuropsychology or specialized rehab. Including chiropractic in the rehab team is supported in multidisciplinary models. (Chiropractic & Manual Therapies, 2018). BioMed Central
-
Return-to-life milestones: sustained symptom control at work/school, restored sleep routine, improved exercise tolerance, and stable mood.
Red flags you should never ignore
Seek urgent care or call emergency services if you notice: worsening headache, repeated vomiting, unequal pupils, seizure, weakness/numbness, slurred speech, confusion, hard-to-wake state, or clear fluid from nose/ears. (BrainLine, 2018; Mayo Clinic, n.d.). BrainLine+1
How thorough questions make the diagnosis
A complete history increases the chance you’ll link the injury with the right symptoms. For example:
-
Taste or smell changes ? often overlooked but common after TBI. (BrainLine, 2018; Fisher Stark, 2021). BrainLine+1
-
Irritability + sleep trouble ? can mask as stress or burnout; track onset after the injury. (U.S. Air Force, 2017; BrainLine, 2018). Hanscom Air Force Base+1
-
Headache with neck stiffness ? check for cervicogenic triggers from whiplash that magnify dizziness and light sensitivity. (Denver Chiropractic, n.d.). Denver Integrated Spine Center
-
“Slow brain” or word-finding ? document with simple cognitive screens and repeat over time. (BrainLine, 2018). BrainLine
Because these patterns are often subtle and delayed, a recheck at 1–2 weeks is crucial to catch what the first visit might miss. (BrainLine, 2018). BrainLine
How integrative care supports recovery
Musculoskeletal and vestibular focus (chiropractic)
-
Reduces neck-driven headaches and dizziness triggers.
-
Restores joint motion and soft-tissue health to ease sensory overload.
-
Adds progressive balance and gaze training to rebuild confidence.
These actions complement medical care and often help patients return to daily life sooner. (Denver Chiropractic, n.d.; NWHSU, n.d.). Denver Integrated Spine Center+1
Medical and whole-person focus (nurse practitioner)
-
Coordinates imaging and specialty referrals, monitors for complications, and manages medications.
-
Coaches sleep, hydration, nutrition, pacing, and mood-support strategies.
-
In higher-acuity settings, follow nursing interventions that reduce secondary injury risks—neuromonitoring, temperature and oxygen checks, and family education. (Figueiredo et al., 2024). MDPI
Together, this plan targets the nervous system and the body’s support systems (sleep, stress, neck mechanics, balance)—a combination linked to better function and a safer return to normal routines. (Chiropractic & Manual Therapies, 2018; U.S. Air Force, 2017). BioMed Central+1
Sample integrative care plan (illustrative)
-
Weeks 0–1
-
Relative rest; limit screen glare; short, quiet walks as tolerated; hydration; gentle neck range-of-motion; symptom diary. (U.S. Air Force, 2017). Hanscom Air Force Base
-
-
Weeks 1–3
-
Chiropractic: light joint/soft-tissue care; posture drills; eye-head coordination basics.
-
NP: reassess red flags; consider MRI if atypical; manage sleep and headache meds; start graded return-to-work plan. (Mayo Clinic, n.d.). Mayo Clinic
-
-
Weeks 3+
-
Progress vestibular/balance training; targeted neck strengthening; timed work/screen intervals, and relaxation practice.
-
Add neuropsych or specialized rehab if progress stalls; keep team communication tight. (Chiropractic & Manual Therapies, 2018). BioMed Central
-
Some clinics also emphasize circulation and lifestyle coaching as part of a holistic approach to recovery. (Pinnacle Health Chiropractic, n.d.; Northwest Florida Physicians Group, n.d.). Pinnacle Health Chiropractic+1
Three quick mistakes to avoid
-
Waiting for symptoms to “prove it.” Mild TBIs are often delayed and subtle; act on patterns linked to the injury. (BrainLine, 2018). BrainLine
-
Ignoring the neck. Cervical dysfunction can drive headaches, dizziness, and visual strain. (Denver Chiropractic, n.d.). Denver Integrated Spine Center
-
Stopping care too soon. Team-based rehab helps persistent cases keep improving across systems. (Chiropractic & Manual Therapies, 2018). BioMed Central
Take-home message
Traumatic brain injuries are easy to miss because many symptoms hide in daily life—concentration lapses, mood shifts, sleep changes, and subtle sensory losses. A thorough history, a focused exam, and tiered testing reveal the pattern. Pairing chiropractic care (for neck, balance, and sensorimotor rehab) with nurse practitioner oversight (for medical safety, sleep, mood, and return-to-life planning) gives patients a practical, whole-person path to recovery. (BrainLine, 2018; Mayo Clinic, n.d.; U.S. Air Force, 2017; Chiropractic & Manual Therapies, 2018; Figueiredo et al., 2024; Jimenez, n.d.). El Paso, TX Doctor Of Chiropractic+5BrainLine+5Mayo Clinic+5
References
BrainLine. (2018, July 6). [Symptoms of traumatic brain injury (TBI)]. www.brainline.org/article/symptoms-traumatic-brain-injury-tbi BrainLine
Chiropractic & Manual Therapies. (2018). [Chiropractic in multidisciplinary rehabilitation teams]. chiromt.biomedcentral.com/articles/10.1186/s12998-018-0200-4 BioMed Central
Denver Chiropractic. (n.d.). [Mild traumatic brain injury: Can a chiropractor help?] denver-chiropractic.com/mild-traumatic-brain-injury-can-chiropractor-help/ Denver Integrated Spine Center
Figueiredo, R., Castro, C., & Fernandes, J. B. (2024). [Nursing interventions to prevent secondary injury in critically ill patients with traumatic brain injury: A scoping review]. Journal of Clinical Medicine, 13(8), 2396. www.mdpi.com/2077-0383/13/8/2396 MDPI
Fisher Stark, P.A. (2021, January 23). [Hidden signs of a serious head injury (traumatic brain injury symptoms)]. fisherstark.com/hidden-signs-of-a-serious-head-injury-traumatic-brain-injury/ Fisher Stark P.A.
HML Functional Care. (n.d.). [How chiropractic neurology supports brain healing]. hmlfunctionalcare.com/how-chiropractic-neurology-supports-brain-healing/ HML Functional Care
Jimenez, A. (n.d.). [El Paso’s premier chiropractic clinic | Injury Medical Pain Treatment Clinic]. dralexjimenez.com/ El Paso, TX Doctor Of Chiropractic
Mayo Clinic. (n.d.). [Traumatic brain injury — Symptoms & causes]. www.mayoclinic.org/diseases-conditions/traumatic-brain-injury/symptoms-causes/syc-20378557 Mayo Clinic
Northwest Florida Physicians Group. (n.d.). [Using chiropractic care to treat traumatic brain injuries]. www.northwestfloridaphysiciansgroup.com/using-chiropractic-care-to-treat-traumatic-brain-injuries Northwest Florida Physicians Group
NWHSU (Northwestern Health Sciences University). (n.d.). [Chiropractic and traumatic brain injuries]. www.nwhealth.edu/news/reis-writes-for-chiropractic-economics-chiropractic-and-traumatic-brain-injuries/ Northwestern Health Sciences University
Pinnacle Health Chiropractic. (n.d.). [Six ways chiropractic care supports healing after TBI]. www.pinnaclehealthchiro.com/blog/six-ways-chiropractic-care-supports-healing-after-tbi/ Pinnacle Health Chiropractic
U.S. Air Force (Hanscom AFB). (2017, March 17). [TBI recognition critical to treating invisible wounds]. www.hanscom.af.mil/News/Article-Display/Article/1126278/tbi-recognition-critical-to-treating-invisible-wounds/ Hanscom Air Force Base
Apex Chiropractic. (2022, August 18). [3 benefits of chiropractic care following a traumatic brain injury]. apexchiroco.com/auto-injury/3-benefits-of-chiropractic-care-following-a-traumatic-brain-injury/ Apex Chiropractic
Disclaimers
Professional Scope of Practice *
The information herein on "Missed Signs of Traumatic Brain Injury Explained" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's wellness blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-C) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on dralexjimenez.com, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card