
For individuals with cervical arthritis, can physical therapies help manage symptoms and bring pain relief?
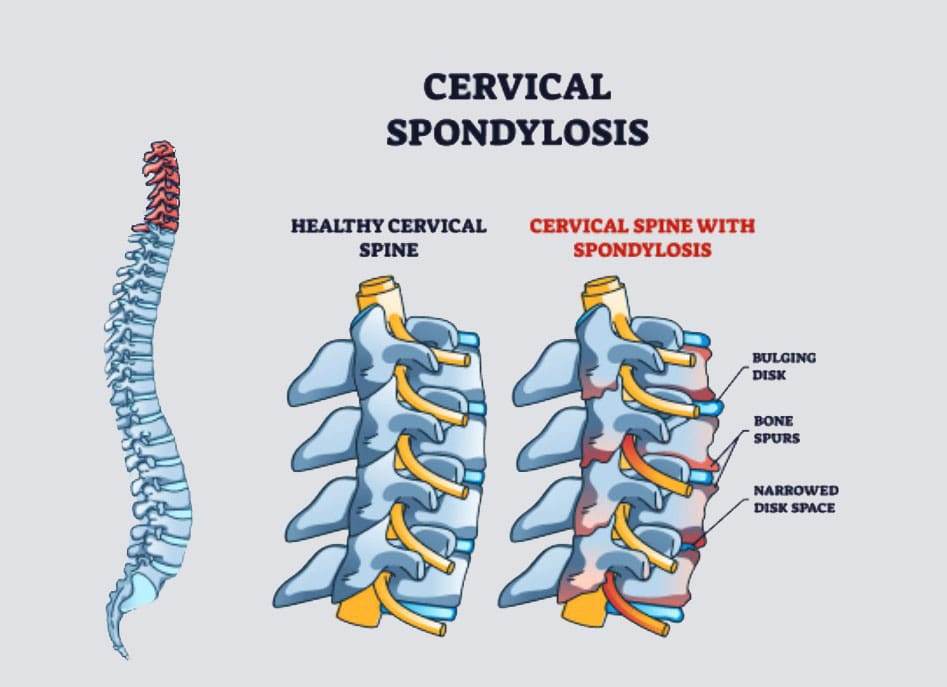
Table of Contents
Cervical Arthritis
Cervical spondylosis, more commonly known as cervical arthritis or arthritis of the neck, refers to the wearing down of neck bones, discs, tendons, ligaments, and joints. The primary symptoms are neck pain and stiffness. However, it is also possible to have cervical spondylosis and not have any symptoms. The condition affects over 85% of individuals over age 65. (American Academy of Orthopaedic Surgeons, 2021) Treatment can consist of conservative therapies and includes physical therapies, alternative medicine therapies, at-home self care, and over-the-counter and prescription medications. Severe cases of cervical spondylosis are treated with surgery to repair damaged parts of the spine.
Symptoms
Neck pain and headaches at the back of the head are usually the first symptoms. (Kazeminasab S. et al., 2022) The neck can also feel stiff, with worse morning symptoms that improve throughout the day. (Johns Hopkins Medicine, 2024) Symptoms can range from mild discomfort to severe pain. As cervical spondylosis progresses, individuals can experience:
- Inability to turn the head or bend the neck.
- A clicking or grinding noise when turning the neck.
- Tenderness with pressure on the neck.
- Pain that radiates to the shoulders or shoulder blades.
- Pain and symptoms that disrupt sleep, sometimes causing waking up throughout the night.
- Symptoms that decrease with rest.
More severe symptoms include:
Cervical Bone Spurs – Osteophytes
Some with cervical spondylosis have bony growths that can place pressure on the spinal nerves (a pinched nerve) (Bon Secours, 2024). Compression of spinal nerve roots produces cervical radiculopathy, which leads to pain, tingling, and weakness that radiates into the shoulders, arms, and hands.
Cervical Myelopathy
This refers to spinal impingement that leads to spinal cord dysfunction. (Spinal cord dysfunction is a nervous system disorder with interruptions in the spinal cord’s motor, sensory, and autonomic functions.) Symptoms include pain, tingling, numbness, muscle spasms, and weakness in areas below the neck. Spinal cord dysfunction can affect mobility, hand use, and bladder or bowel function control.
Causes
Where degenerative changes are commonly associated with cervical spondylosis, other conditions, and factors can lead to it and include:
Autoimmune Diseases
- Rheumatoid arthritis and psoriatic arthritis can cause chronic inflammation in the cervical spine.
Trauma
- Neck trauma, including injury and repetitive stress on the neck.
- Cervical spondylosis is commonly seen in occupations that involve neck-stressing activities, such as sports.
Age
- Wearing down of the spinal discs cartilage between the vertebrae.
- Developing cervical spondylosis increases with age, especially after 40. (Kazeminasab S. et al., 2022)
Genetics
- Genetic components have been identified in connection with cervical spondylosis, meaning that some types of arthritis that lead to spinal damage are hereditary. (Kazeminasab S. et al., 2022)
Treatment
Treatment begins conservatively, using protocols to preserve function and avoid surgery. Nonsurgical treatments include medications, physical therapy, at-home exercises, and alternative medicine. The treatment method a healthcare provider chooses will depend on how severe the spondylosis is and other factors like age, how much pain is being experienced, the cause, and overall health. The main objectives are to relieve pain, prevent long-term damage to the spinal cord and nerves, and help maintain performing daily activities. (Bon Secours, 2024)
Medications
Medicines used to treat cervical spondylosis include:
Nonsteroidal Anti-inflammatory Drugs NSAIDs
- NSAIDs, including ibuprofen and naproxen sodium, are available without a prescription to relieve pain and inflammation.
- A healthcare provider can prescribe a more powerful NSAID to help manage severe symptoms.
Corticosteroids
- A corticosteroid injection or a short course of an oral corticosteroid, like prednisone, can ease pain and reduce inflammation.
Muscle Relaxants
- If cervical spondylosis causes muscle spasms, a healthcare provider can prescribe cyclobenzaprine, a muscle relaxant, to manage symptoms.
Antidepressants
- Some types of antidepressants can ease neck pain from cervical spondylosis.
Anti-seizure Meds
- Some anti-seizure drugs can cause nerve pain resulting from damaged nerves.
Physical Therapies
- Physical therapy will help manage pain and stiffness and keep muscles loose and relaxed.
- A physical therapist will teach the patient exercises to stretch and strengthen neck and shoulder muscles.
At-Home Self Care
At-home exercises can help relieve pain, stiffness, and swelling. Some can include:
- Reducing inflammation and stress on the neck through posture training.
- At-home targeted stretches and exercises will help bring pain relief.
- Ice treatment reduces swelling.
- Heat will increase circulation.
- A neck brace may be recommended briefly to avoid muscle weakness and stiffness.
Alternative Medicine
- Chiropractic adjustments and massage therapy are alternative treatments that will help manage cervical spondylosis.
- Chiropractic adjustments can relieve neck pain and stiffness. (American Chiropractic Association, 2024)
- X-rays are done before to ensure it is safe. (Jenkins H. J. et al., 2018)
- Acupuncture can also be beneficial in reducing neck pain and increasing energy circulation. (Gu C. L. et al., 2019)
- Various therapeutic massage therapies will help relieve neck pain and stiffness. Talk to a healthcare provider before starting treatment so they can advise on whether neck massages are safe.
Surgery
A healthcare provider may recommend surgical treatment when all other treatments have failed, if neurological symptoms are severe, or if neck arthritis causes extreme pain or disability. Surgery to treat cervical spondylosis can involve removing bone spurs, part of the cervical vertebra, or a herniated disc. The removed portions of the cervical spine are fused with hardware and bone grafts.
Injury Medical Chiropractic and Functional Medicine Clinic
Chiropractic therapy is among the more conservative treatment options and may be tried first before proceeding with surgery. Injury Medical Chiropractic and Functional Medicine Clinic works with primary healthcare providers and specialists to develop an optimal health and wellness solution.
Arthritis Explained
References
American Academy of Orthopaedic Surgeons. (2021). Cervical spondylosis (arthritis of the neck). orthoinfo.aaos.org/en/diseases–conditions/cervical-spondylosis-arthritis-of-the-neck/
Kazeminasab, S., Nejadghaderi, S. A., Amiri, P., Pourfathi, H., Araj-Khodaei, M., Sullman, M. J. M., Kolahi, A. A., & Safiri, S. (2022). Neck pain: global epidemiology, trends and risk factors. BMC musculoskeletal disorders, 23(1), 26. doi.org/10.1186/s12891-021-04957-4
Johns Hopkins Medicine. (2024). Spinal arthritis (arthritis in the back or neck). www.hopkinsmedicine.org/health/conditions-and-diseases/spinal-arthritis
Bon Secours. (2024). Cervical osteoarthritis (arthritis in the neck). www.bonsecours.com/health-care-services/spine-care/conditions/cervical-osteoarthritis
American Chiropractic Association. (2024). Neck pain. www.acatoday.org/patients/neck-pain-and-chiropractic/
Jenkins, H. J., Downie, A. S., Moore, C. S., & French, S. D. (2018). Current evidence for spinal X-ray use in the chiropractic profession: a narrative review. Chiropractic & manual therapies, 26, 48. doi.org/10.1186/s12998-018-0217-8
Gu, C. L., Yan, Y., Zhang, D., & Li, P. (2019). An evaluation of the effectiveness of acupuncture with seven acupoint-penetrating needles on cervical spondylosis. Journal of pain research, 12, 1441–1445. doi.org/10.2147/JPR.S199798
Disclaimers
Professional Scope of Practice *
The information herein on "Living with Cervical Arthritis: Coping Strategies and Self-Care Tips" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's wellness blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-C) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on dralexjimenez.com, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card






