Table of Contents
TBI Toxicity and Whole-Body Healing: An Integrative Guide for People Recovering from Car Crashes, Sports Concussions, and Workplace Head Injuries

Key Takeaway
After the initial hit, the brain can stay in a “toxic storm” for days to weeks. That storm includes excitotoxicity (glutamate and calcium overload), oxidative stress (excessive reactive oxygen species), neuroinflammation (overactivation of microglia and the immune system), disruption of the blood-brain barrier (BBB), cerebral edema (swelling), and alterations to the gut-brain axis that can exacerbate inflammation. A whole-body plan—medical triage plus integrative care (chiropractic, supervised exercise, vestibular and cervical rehab, sleep and nutrition, and gut support)—helps calm the storm and guide the nervous system back toward balance (homeostasis) for the long haul (Priester, 2025; Jassam et al., 2017; Salehi et al., 2017). News and Events+2PMC+2
Part 1 — What Makes TBIs “Toxic” After the Impact?
1) Excitotoxicity: when “too much signal” hurts cells
Right after injury, damaged neurons can dump large amounts of glutamate, the brain’s main excitatory neurotransmitter. Neighboring cells then allow in too much calcium, triggering enzymes that break down proteins, lipids, and DNA. This process is known as excitotoxicity, and it can cause the death of otherwise healthy cells surrounding the original injury site. It’s a major “secondary injury” pathway that unfolds minutes to days after impact (Raghupathi, 2004; Charlie Waters Law, n.d.). PubMed+1
Why it matters to you: Symptoms can worsen or change over several days, even when the scan on day one looked “normal.” Your care team should closely monitor you during this period.
2) Oxidative stress: reactive oxygen species (ROS) pile up
Inflammation, mitochondrial strain, and lipid peroxidation generate ROS that damage membranes, receptors, and DNA. Antioxidant defenses (like Nrf2-regulated genes) may be overwhelmed. Reviews indicate that oxidative stress is a key driver of secondary damage and subsequent cognitive problems, and antioxidant-support strategies are currently under active investigation (Fesharaki-Zadeh, 2022; Wu et al., 2022). MDPI+1
Why it matters: Sleep, nutrition, and targeted rehab are not “extras.” They can help your own antioxidant systems work better while you heal.
3) Neuroinflammation: microglia help—and can harm—over time
Microglia (the brain’s resident immune cells) rush in to clean debris and can release helpful anti-inflammatory and growth factors early on. But if activation persists or becomes excessive, microglia release cytokines and oxidative molecules that damage nearby tissue and may contribute to long-term neurodegeneration (Denniss et al., 2023; Jassam et al., 2017). PMC+1
Why it matters: Ongoing headaches, brain fog, or mood changes weeks to months later may reflect lingering neuroinflammation—not “all in your head.” Timely, steady rehab matters.
4) Blood-brain barrier (BBB) disruption and cerebral edema
The BBB can become leaky after TBI. When tight junctions loosen, plasma proteins and water move into the tissue, worsening swelling (vasogenic edema). At the cellular level, failed ion pumps cause water to rush into cells (cytotoxic edema). Both increase pressure and reduce oxygen delivery (Salehi et al., 2017). PMC
Why it matters: Elevating the head of the bed, watching sodium and hydration under medical guidance, and following your clinician’s instructions on activity can protect a vulnerable brain during this phase.
5) The gut-brain axis: why the stomach feels the hit
TBIs can slow intestinal movement, increase gut permeability, and shift the microbiome. This “gut dysbiosis” can send inflammatory signals back to the brain, exacerbating neuroinflammation and symptoms such as fatigue and brain fog (Cannon et al., 2023; Celorrio et al., 2021; Bansal et al., 2009). Families often notice appetite changes, reflux, constipation/diarrhea, or food sensitivities after a concussion or head injury. PMC+2PMC+2
Why it matters: Gut care is brain care. Feeding the microbiome and reducing gut inflammation can support the brain’s recovery.
Part 2 — How Long Do Toxic Effects Last?
New research confirms the secondary injury phase can extend for weeks. A Missouri S&T summary (republished from The Conversation) shows antioxidant materials targeted ROS and lipid peroxidation products in mouse TBI models, improving recovery (Priester, 2025). While early human trials are still ahead, the message is clear: countering persistent biochemical fallout may improve long-term outcomes. News and Events
Clinical picture: With time and support, the nervous system can re-regulate. But many people need structured, multi-system care for weeks to months, especially after car crashes, sports concussions, or workplace head injuries.
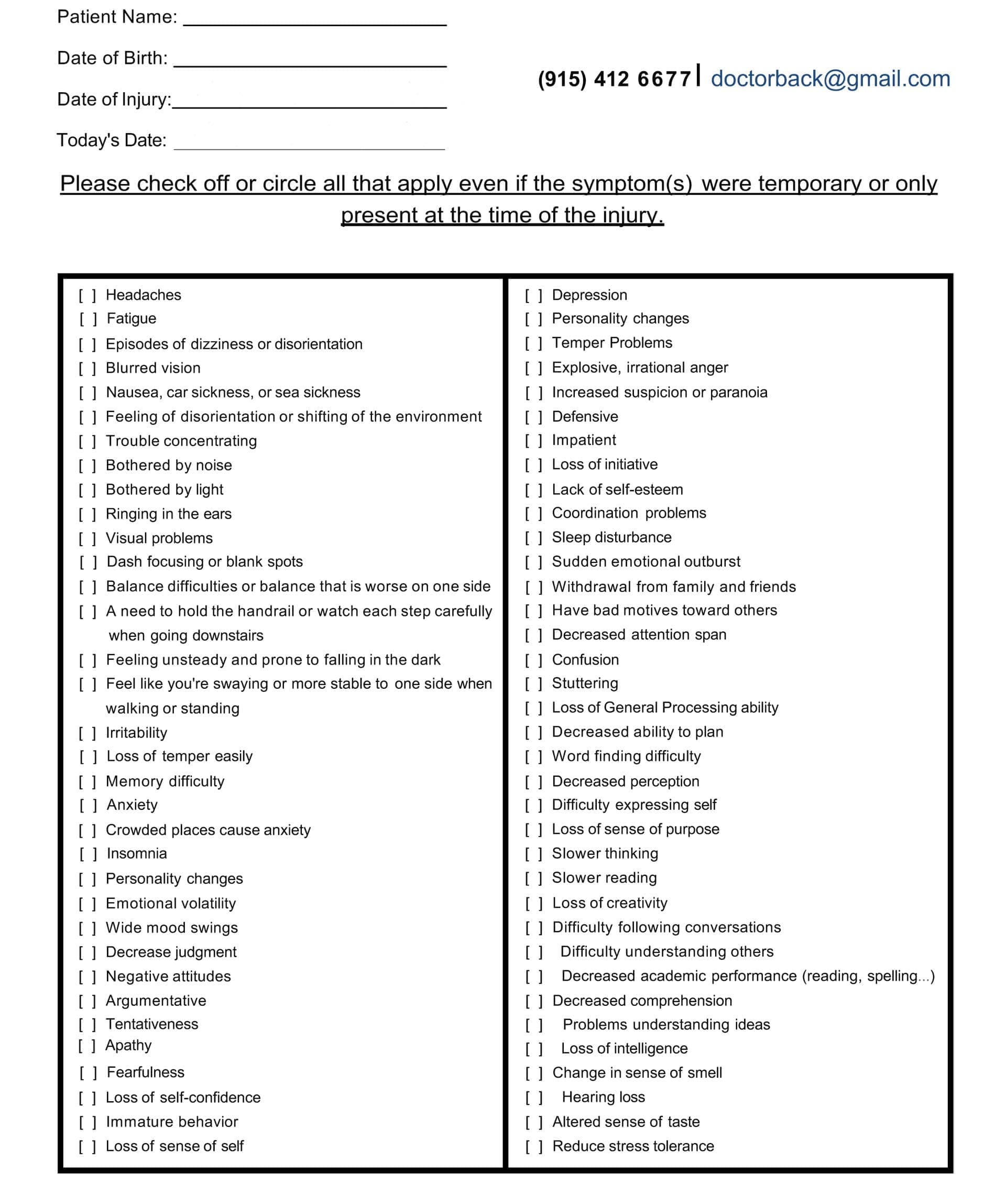
Symptom Questionnaire:
Part 3 — An Integrative Care Map Led by Chiropractic Nurse Practitioners (CNPs)
Chiropractic Nurse Practitioners (CNPs) bridge the gap between medical and musculoskeletal care. In our region, Dr. Alexander Jimenez, DC, APRN, FNP-BC, emphasizes dual-scope assessment, advanced imaging when appropriate, careful cervical and vestibular evaluation, graded movement, and nutrition/gut strategies to reduce inflammation and support healing. He coordinates with neurologists, primary care, physical therapy, and neuropsychology to build patient-specific plans (Jimenez, n.d.). Invalid URL
Below is a practical, step-by-step plan that you can share with your care team. It is organized for three common scenarios—car accidents, sports concussions, and workplace head injuries—but the core ideas overlap.
Step 1 — Acute triage and red flags (all settings)
-
Go to the ER for red flags: worsening headache, repeated vomiting, seizures, unequal pupils, weakness/numbness, speech difficulty, severe neck pain, or any rapidly changing symptoms. Follow imaging and medication guidance.
-
Protect sleep on the first nights, but follow your clinician’s monitoring advice.
-
Pain control should avoid sedating or constipating regimens where possible. Ask about non-opioid options and simple positioning.
Why CNP leadership helps: CNPs track neuro and musculoskeletal status together—watching for post-concussive signs and cervical sprain/strain patterns that worsen dizziness or headaches.
Step 2 — Calm the toxic cascade
Target excitotoxicity & oxidative stress (supportive measures):
-
Early activity pacing (not full bed rest): brief, light movement as tolerated—short walks, gentle range of motion exercises, and breathwork to reduce sympathetic overdrive.
-
Nutrition: emphasize omega-3–rich fish, colorful vegetables and berries, olive oil, nuts, seeds, and adequate protein. These foods support Nrf2-driven antioxidant responses and may help reduce oxidative stress (Wu et al., 2022; Fesharaki-Zadeh, 2022). PMC+1
-
Hydration and electrolyte balance, under the guidance of a clinician, support perfusion and help manage the risk of brain swelling.
What your CNP may add: a medication/supplement review (to avoid excess sedatives) and coordinated referrals (neurology, vestibular rehab, and vision therapy) when needed.
Step 3 — Stabilize the neck, balance systems, and vision
Why the neck matters: Cervical joint dysfunction and soft tissue strain can amplify headaches, dizziness, and visual motion sensitivity. Gentle, graded cervical mobilization, soft-tissue therapy, and posture training can ease neck-driven inputs to the vestibular system. In many clinics, chiropractors report improvements in neck pain and cervicogenic dizziness when cervical alignment and motion are restored with careful, individualized techniques (clinical observations; see also integrative chiropractic discussions). Invalid URL
Vestibular/oculomotor rehab:
-
Gaze stabilization (VOR) drills, smooth pursuit and saccade practice, and graded exposure to head/eye movements.
-
Balance progressions: firm or foam surfaces, eyes open or closed, dual-task layers.
Why CNP leadership helps: CNPs can integrate cervical, vestibular, and vision care to keep symptoms below threshold and advance safely week by week.
Step 4 — Heal the gut-brain axis
What changes after TBI: slowed transit, increased permeability, and microbial shifts can feed back into the brain’s inflammation (Cannon et al., 2023; Celorrio et al., 2021). PMC+1
Gut-support basics your team may use:
-
Fiber and polyphenols: berries, leafy greens, beans, and extra-virgin olive oil.
-
Prebiotic foods: oats, onions/garlic, asparagus, and bananas.
-
Probiotics/fermented foods as tolerated (e.g., yogurt, kefir, kimchi).
-
Gentle motility supports include hydration, magnesium-rich foods, and regular physical activity, such as walking.
-
Trigger review: identify foods that worsen reflux, bloating, or stools.
-
Medication check: discuss NSAIDs or other meds that may affect the gut.
Outcome goal: reduce gut-derived inflammation to lighten the brain’s inflammatory load.
Step 5 — Sleep, stress, and autonomic reset
Sleep is a primary antioxidant and a key tool for neuroplasticity. Aim for 7–9 hours, consistent timing, a dark, cool room, and a wind-down routine. Breathing drills, such as slow nasal breathing (4-6 breaths/min), and brief daytime sunlight cues help regulate the circadian rhythm and the autonomic nervous system, also known as the “fight/flight” response.
Why CNP leadership helps: CNPs can blend conservative care with sleep hygiene, medication timing, and gentle HRV-oriented practices to improve resilience.
Step 6 — Graded aerobic and strength training
After receiving medical clearance, initiate sub-symptom aerobic activity (e.g., brisk walking or stationary cycling) that keeps symptoms at < 2/10. Add scapular/cervical stabilizers, hip/leg strength, and mobility flows. Movement boosts blood flow, supports mitochondrial function, and often improves mood and sleep, which in turn reduces neuroinflammation.
Step 7 — Cognitive and mood support
Short, frequent “cognitive reps” (timed focus blocks followed by rest), task lists, and a gentle return to school/work with accommodations can reduce overload. If mood symptoms persist (irritability, anxiety, depression), early referral to behavioral health is smart—neuroinflammation can affect mood circuits, and multidisciplinary support speeds recovery (Schimmel et al., 2017). PMC
Part 4 — Tailored Paths by Scenario
A) Car accidents (MVCs)
Common pattern: mixed TBI + whiplash + whole-body stress.
Priorities:
-
Rule out serious injury; follow imaging and medication plans.
-
Cervical care (gentle mobilization/adjusting when appropriate), soft-tissue work, and posture drills to calm cervicogenic headaches and dizziness.
-
Vestibular/vision care if motion or screens trigger symptoms.
-
Gut reset (fiber, polyphenols, and probiotics as tolerated) because pain meds and stress slow transit.
-
Pace the return to driving: start with very short, low-traffic routes and daylight only; build up slowly.
B) Sports concussions
Common pattern: exertion intolerance, visual motion sensitivity, and neck strain.
Priorities:
-
Return-to-play protocols with CNP oversight and athletic training support.
-
Sub-symptom cardio and dual-task balance to rebuild tolerance.
-
Cervical and vestibular integration allows the system to relearn coordinated head-eye-body movement.
-
Nutrition: adequate energy and protein; limit alcohol; prioritize sleep for plasticity.
C) Workplace head injuries
Common pattern: variable severity; physical and cognitive load at work.
Priorities:
-
Job-specific accommodations (lighting, screen breaks, reduced noise).
-
Functional capacity rebuilding with graded loads.
-
Stress management techniques (such as breathing exercises, pacing, and micro-breaks) can help avoid flare-ups.
-
Team communication: CNPs often liaise with HR and safety to ensure a safe return-to-duty process.
Part 5 — What the Evidence Says About “Toxicity” and Long-Term Risk
-
Weeks-long biochemical fallout: Secondary cascades—excitotoxicity, neuroinflammation, and ROS—can persist and are linked to later neurodegeneration; antioxidant strategies are being developed (Priester, 2025; Fesharaki-Zadeh, 2022; Wu et al., 2022). News and Events+2MDPI+2
-
Microglia: double-edged sword: Helpful early, harmful when overactive; chronic activation correlates with ongoing symptoms (Denniss et al., 2023; Jassam et al., 2017). PMC+1
-
Vascular/BBB and edema: BBB leakage, along with both cytotoxic and vasogenic edema, drives pressure problems and tissue loss (Salehi et al., 2017). PMC
-
Gut-brain axis: TBI slows transit, increases permeability, and shifts microbiota; gut-directed care can be part of the plan (Cannon et al., 2023; Celorrio et al., 2021; Bansal et al., 2009). PMC+2PMC+2
Part 6 — Putting It Together: A 12-Week Recovery Blueprint You Can Personalize With Your CNP
Weeks 0–2 (Protect & Stabilize)
-
Medical follow-up; watch for red flags.
-
Gentle mobility, short walks, and breath work.
-
Anti-inflammatory plate: colorful produce, olive oil, fish, nuts; hydrate.
-
Sleep schedule, screen dimming, and noise control.
-
If dizziness or neck pain persists, begin cervical + vestibular care.
Weeks 3–4 (Sub-Symptom Rebuild)
-
Add 15–20 minutes of easy cardio daily (symptom-capped).
-
Begin gaze and balance drills; light resistance for scapular/neck stabilizers.
-
Fiber + fermented foods; magnesium-rich foods for motility.
Weeks 5–8 (Tolerance & Skill)
-
Progress cardio and strength; add dual-task balance.
-
Tighten sleep and stress routines; small exposure to triggers (busy stores, screens) with breaks.
Weeks 9–12 (Return to Role)
-
Sport- or job-specific drills; staged return to duty/play.
-
Keep the gut-brain support diet; review supplements/meds with your CNP.
-
Re-screen cognition, balance, and cervical function to adjust the plan.
Part 7 — How Families and Care Teams Can Help
-
Track wins: short logs of sleep, steps, and symptom scores help guide progress.
-
Guard the routine: consistent meals, daylight, gentle activity, and a regular bedtime are powerful medicines.
-
Lower “noise”: reduce extra appointments and screens on flare days.
-
Cheer the small steps: brain recovery is rarely linear—expect positive and “off” days.
-
Stay coordinated: let your CNP quarterback the plan with the rest of the team.
Clinical Perspective from Dr. Alexander Jimenez, DC, APRN, FNP-BC
Dr. Jimenez’s dual-scope approach emphasizes careful cervical assessment (since neck dysfunction can exacerbate dizziness and headaches), vestibular and oculomotor testing, graded exercise, and a comprehensive approach to nutrition and gut support for persistent symptoms. He emphasizes that coordinated, stepwise care helps mitigate excitotoxicity and oxidative stress indirectly by normalizing movement, sleep, and autonomic tone, while reducing gut-driven inflammatory load—an approach that aligns with current secondary injury science. Invalid URL
Bottom Line
TBI is more than a one-time event. It is an injury plus a cascade. Addressing the cascade—with smart medical care and whole-body integrative steps—gives the brain its best chance to heal. A Chiropractic Nurse Practitioner can help you blend cervical and vestibular rehab, sleep and stress resets, nutrition and gut care, and gradual return-to-life practices into one clear path.
References
Bansal, V., Costantini, T., Ryu, S. Y., Peterson, C., Loomis, W., Eliceiri, B., Baird, A., & Coimbra, R. (2009). Traumatic Brain Injury and Intestinal Dysfunction. Journal of Neurotrauma, 26(8), 1353–1359. pmc.ncbi.nlm.nih.gov/articles/PMC2989839/ PMC
Cannon, A. R., et al. (2023). Traumatic brain injury induced inflammation and GI motility. Frontiers in Immunology. pmc.ncbi.nlm.nih.gov/articles/PMC10065904/ PMC
Celorrio, M., et al. (2021). Gut-brain axis in traumatic brain injury: Impact on microbiome. Cells. pmc.ncbi.nlm.nih.gov/articles/PMC8552843/ PMC
Denniss, R. J., et al. (2023). Brain trauma and the secondary cascade in humans. Frontiers in Neurology. pmc.ncbi.nlm.nih.gov/articles/PMC10215746/ PMC
Fesharaki-Zadeh, A. (2022). Oxidative stress in traumatic brain injury. International Journal of Molecular Sciences, 23(21), 13000. www.mdpi.com/1422-0067/23/21/13000 MDPI
Jassam, Y. N., Izzy, S., Whalen, M., McGavern, D. B., & El Khoury, J. (2017). Neuroimmunology of traumatic brain injury. Neuron, 95(6), 1246–1265. pmc.ncbi.nlm.nih.gov/articles/PMC5678753/ PMC
Priester, A. (2025, May 22). Traumatic brain injuries have toxic effects that last weeks after initial impact ? an antioxidant material reduces this damage in mice. Missouri S&T News (republished from The Conversation). news.mst.edu/2025/05/traumatic-brain-injuries-have-toxic-effects-that-last-weeks-after-initial-impact-%E2%88%92-an-antioxidant-material-reduces-this-damage-in-mice/ News and Events
Raghupathi, R. (2004). Cell death mechanisms following traumatic brain injury. Neurosurgical Focus, 16(6). pubmed.ncbi.nlm.nih.gov/15193035/ PubMed
Salehi, A., Zhang, J. H., & Obenaus, A. (2017). Response of the cerebral vasculature following traumatic brain injury. Journal of Cerebral Blood Flow & Metabolism, 37(7), 2320–2339. pmc.ncbi.nlm.nih.gov/articles/PMC5531360/ PMC
Wu, A. G., et al. (2022). Targeting Nrf2-mediated oxidative stress response in TBI. Biomedicines, 10(3), 520. pmc.ncbi.nlm.nih.gov/articles/PMC9001080/ PMC
Zhu, C.-S., et al. (2018). A review of traumatic brain injury and the gut microbiome. Brain Sciences, 8(6), 113. pmc.ncbi.nlm.nih.gov/articles/PMC6025245/ PMC
Additional context and clinical observations
Jimenez, A. (n.d.). Injury Medical & Chiropractic / Dr. Alex Jimenez. dralexjimenez.com/ Invalid URL
Charlie Waters Law. (n.d.). Excitotoxicity: A Secondary Injury in Traumatic Brain Damage. www.charliewaterslaw.com/brain-injury/excitotoxicity-a-secondary-injury-in-traumatic-brain-damage/ Charlie Waters Law
Disclaimers
Professional Scope of Practice *
The information herein on "TBI Toxicity and Whole-Body Healing for Recovery" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's wellness blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-C) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on dralexjimenez.com, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card