Table of Contents
Introduction
The gut system makes sure that the good bacteria is helping the gut by digesting the consumed food into nutrients for the body and keeping the unwanted pathogens from causing chronic inflammation to the intestinal permeability barrier. The gut has a pretty good bidirectional connection to the brain as they send signals back and forth to each other while making sure that the body is functional and that everything is working properly. In this 2 part series, we will be taking at what is the gut-brain axis and how does it function in the body. Part 2 will be taking at the different factors that can affect the gut-brain axis. By referring patients to qualified and skilled providers who specialized in gastroenterology services. To that end, and when appropriate, we advise our patients to refer to our associated medical providers based on their examination. We find that education is the key to asking valuable questions to our providers. Dr. Alex Jimenez DC provides this information as an educational service only. Disclaimer
Can my insurance cover it? Yes, in case you are uncertain here is the link to all the insurance providers we cover. If you have any questions, please call Dr. Jimenez at 915-850-0900.
What Is The Gut-Brain Axis?
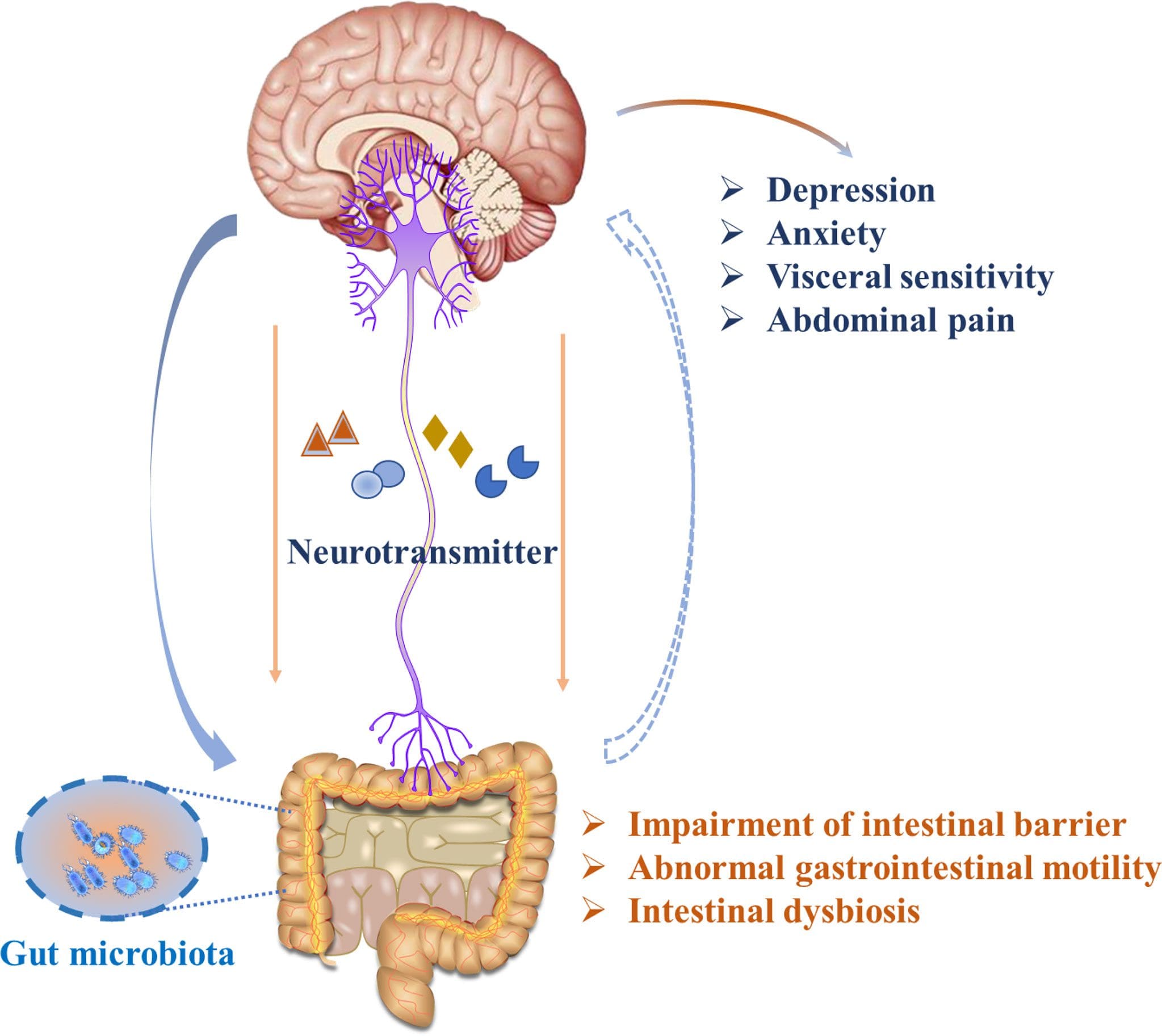
Also known as the “gut feeling” in the body, the gut-brain axis as research shows that the gut-brain axis has consisted of bidirectional communication between the central and enteric nervous system. The brain sends signals to the gut to make sure that everything is working properly and vice versa. Other studies have also shown that gut microbes actually communicate to the central nervous system through at least 3 parallel interactive channels that include the nervous, endocrine, and immune signaling mechanisms that make the body functional. When the gut or the brain is being dysfunctional, it can cause many problems in the body and can be developed into chronic issues that will happen over time.
The “Forgotten Organ”
Research studies have shown that the intestinal microflora is a positive health asset as it is crucially influenced by the normal structural and fundamental development of the mucosal immune system. What this means is that the bacteria density increases in the jejunum/ileum from the stomach and duodenum. In the large intestine, there are colon-residing bacteria that achieve the highest cell densities recorded for any ecosystem, whether it is the gut or the brain. Other studies have shown that the resident microorganisms in the body establish in their respective colonies while performing a variety of vital functions in the body by exerting a range of protective, structural, and metabolic effects on the intestinal mucosa.
HCTP Therapy
Stem cells* or HCTP (human cellular tissue products) are a form of regenerative medicine that both international and nationally affiliated clinics and distribution organizations use to help boost the body’s own natural healing process. HCTP has beneficial properties by repairing cells, diseased organs, and tissues back to their original state and function in the body. With more and upcoming research about the beneficial properties of HCTP, many individuals with either neurological disorders or gut issues can be provided with relief.
Diversity Is The Key For Gut Health
Having diversity in the body is important for gut health as it helps shape a person in the world. The alpha diversity is a measure of the compositional complexity of a community within a site as it increases with the number of present species and with the evenness of their relative abundances in the gut. While the beta diversity looks at the differences in the taxonomic abundance profiles from different samples as presence-absence data are often used to identify which species are shared by samples and which are not. Research studies have shown that the abundance of specific bacterial genera can be significantly predicted by a person’s personality traits. The gut needs bacteria to thrive on the inside as it helps protect the gut from toxins and pathogens that are trying to disturb the microbiota. Other studies have found that when nutritional foods enter the GI microbial ecosystem, it provides macro-and micro-nutrients to the gut microbial as it helps the gut to be diverse, stable, and healthy.
Neurodevelopment & The Gut
Studies have found that the bidirectional communication between the gut and brain is established due to the colonization patterns and cognition at the early stages of a person’s life. The brain is part of the central nervous system that makes sure that the information from the gut is being transferred back to the brain. Other studies have been shown that the production of metabolites can help influence the central nervous system and enhanced the integrity of the intestinal epithelial layer through SCFAs (short-chain fatty acids). The SCFAs traveling back and forth through the gut and the brain allows the bacterial strains will decrease the permeability of the blood-brain barrier.
Microbiota Regulates Anxiety
The gut microbiota actually helps to regulate the body and brain function in the body as it can help monitor the neuron signals that are providing the sensations and emotional signals in the body. Studies have found that when the intestinal flora modulates the gut-brain axis communication, it involves the nervous system, immune system, and endocrine system to make it functional. When the intestinal flora is being affected by pathogens though, it can cause a series of changes in the physical and mental symptoms to occur like anxiety. This is due to any inflammation and dysbiosis that has been affecting the gut, as research studies show that any chronic inflammation has been linked to mental illnesses like anxiety and depression. When a person has inflammation in the gut, it can cause them pain and suffering as they don’t really know what is going on. By establishing antioxidant-riched foods into the gut system, the inflammation can be dampened and even improve brain health.
Conclusion
All in all, the gut-brain axis has a bidirectional connection that makes sure that the gut and the brain are communicating with each other as well as doing their jobs properly. With this bidirectional communication, the gut makes sure that the signaling mechanisms are working properly and that unwanted pathogens are not entering each of the systems. When this happens, both the gut and the brain will begin to be dysfunctional and cause chronic issues to be developed. Utilizing anti-inflammatory foods and exercises can dampen these effects and the individual can begin their life pain-free.
References
Carabotti, Marilia, et al. “The Gut-Brain Axis: Interactions between Enteric Microbiota, Central and Enteric Nervous Systems.†Annals of Gastroenterology, Hellenic Society of Gastroenterology, 2015, www.ncbi.nlm.nih.gov/pmc/articles/PMC4367209/.
Clapp, Megan, et al. “Gut Microbiota’s Effect on Mental Health: The Gut-Brain Axis.†Clinics and Practice, PAGEPress Scientific Publications, Pavia, Italy, 15 Sept. 2017, www.ncbi.nlm.nih.gov/pmc/articles/PMC5641835/.
Heiman, Mark L, and Frank L Greenway. “A Healthy Gastrointestinal Microbiome Is Dependent on Dietary Diversity.†Molecular Metabolism, Elsevier, 5 Mar. 2016, www.ncbi.nlm.nih.gov/pmc/articles/PMC4837298/.
Johnson, Katerina V-A. “Gut Microbiome Composition and Diversity Are Related to Human Personality Traits.†Human Microbiome Journal, Elsevier Ltd, Mar. 2020, www.ncbi.nlm.nih.gov/pmc/articles/PMC8336012/.
Martin, Clair R, et al. “The Brain-Gut-Microbiome Axis.†Cellular and Molecular Gastroenterology and Hepatology, Elsevier, 12 Apr. 2018, www.ncbi.nlm.nih.gov/pmc/articles/PMC6047317/.
O’Hara, Ann M, and Fergus Shanahan. “The Gut Flora as a Forgotten Organ.†EMBO Reports, U.S. National Library of Medicine, July 2006, www.ncbi.nlm.nih.gov/pmc/articles/PMC1500832/.
Rothenberg, Sarah E, et al. “Neurodevelopment Correlates with Gut Microbiota in a Cross-Sectional Analysis of Children at 3 Years of Age in Rural China.†Scientific Reports, Nature Publishing Group UK, 1 Apr. 2021, www.ncbi.nlm.nih.gov/pmc/articles/PMC8016964/.
Seo, Dong-Oh, and David M Holtzman. “Gut Microbiota: From the Forgotten Organ to a Potential Key Player in the Pathology of Alzheimer’s Disease.†The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, Oxford University Press, 18 June 2020, www.ncbi.nlm.nih.gov/pmc/articles/PMC7302187/.
Warner, Barbara B. “The Contribution of the Gut Microbiome to Neurodevelopment and Neuropsychiatric Disorders.†Pediatric Research, U.S. National Library of Medicine, 25 Sept. 2018, pubmed.ncbi.nlm.nih.gov/30283047/.
Yang, Beibei, et al. “Effects of Regulating Intestinal Microbiota on Anxiety Symptoms: A Systematic Review.†General Psychiatry, BMJ Publishing Group, 17 May 2019, www.ncbi.nlm.nih.gov/pmc/articles/PMC6551444/.
Disclaimer
Disclaimers
Professional Scope of Practice *
The information herein on "A Focused Look On The Gut-Brain Axis | Part 1" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's wellness blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-C) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on dralexjimenez.com, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card