
Coronavirus definitely took us all by surprise. With an uncontrollable infection rate, the medical world seemed to forget about the chronic and metabolic diseases. Yes, a true pandemic, more than 440,000 deaths, and a fast-developing disease with no guideline treatment, the medical world did what it had to do. Today, with the new hope that the vaccination program has brought, we can finally take a deep breath, stay home, promote and practice social distancing, and hope for the best. Despite this reality, there is still another disease that is the main cause of mortality in the United States, Cardiovascular disease. Â As a non-transmittable chronic disease, there is no vaccine for this one (and never will be). However, an in-depth medical assessment, lifestyle changes, and monitoring of risk factors can stop and reverse this condition.
However, a lot of things have changed since I went to school. Cardiovascular disease encompassed any dysfunction that would affect the heart and blood vessels, in a broad sense, the circulatory system. Consequently, this definition would leave out all of the metabolic disturbances that come along with cardiovascular disturbances. Indeed, the body works together with all systems, the circulatory system, the skeletal system, the respiratory system, digestive system, endocrine system, renal system, etc. Therefore, when a problem happens in one of them, that same problem can certainly be reflected in other systems.
Nowadays, the Functional Medicine approach seeks to know what promotes lumen stenosis on an artery and how to stop it. What is happening outside of this artery that is affecting the blood pressure? Changing the artery’s ecosystem, modifying what goes around this specific condition is only possible if we include lifestyle changes in our treatment guidelines.
Table of Contents
Lifestyle changes
The EUROASPIRE IV survey, a lifestyle monitory survey, showed that large proportions of patients with high CDV risk were engaging in unhealthy lifestyle habits that would eventually lead to uncontrolled blood pressure, hyperlipidemia, and diabetes.
But how can an unhealthy diet promote a chronic disease? We are just trying to live our best life.
The truth is that diet, how we exercise, what we consume, and how we process stress has a lot to do with this ecosystem.
Standard American diet:
According to the WHO, it is estimated that 1.5 billion people worldwide are overweight, and at least 500 million are obese. Consequently, there has been a rise in obesity-related health problems, including cardiometabolic conditions. Genetic predispositions, physical inactivity, and consumption of a high-fat diet (HFD) can lead to the development of increased fat deposition in our bodies. Recently, a study in mice reported that HFD (40% of total energy), with 12% of saturated fat mimicking the standard American diet (SAD), compared with other HFD with 6% and 24% saturated fat. The study concluded the SAD-mimicking diet led to the greatest adiposity, macrophage infiltration, and insulin resistance (IR).
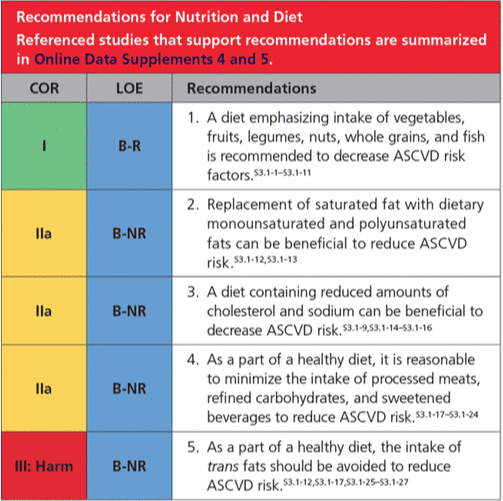
On the same note, ACC/AHA, the risk prevention guideline, determines that plant-based, Mediterranean diet and the dietary introduction of fruit, vegetables, legumes, or animal protein (preferably fish), and fiber are associated with a lower risk of all-cause mortality than SAD.
Nutritional assessment
The assessment of nutritional status included body composition analysis. Body composition analysis should be used to determine if the patient can benefit from weight loss. However, while reducing weight can seem shallow, the true benefits reflect the lower LDL levels, triglyceride, cholesterol, and blood glucose.
Exercise as a risk prevention
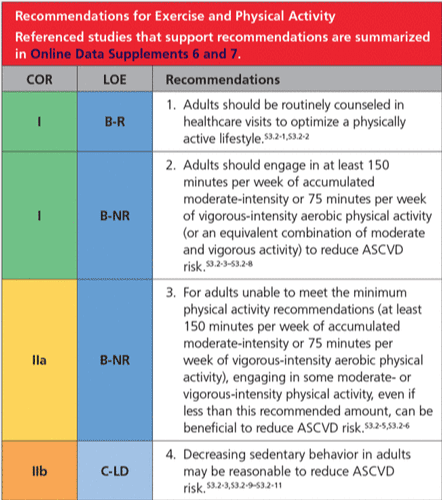
Physical activity is essential for risk prevention, but up until recently, this was not a part of the treatment guidelines. Despite the numerous benefits linked to physical activity and exercise, half of the adult population in the United States does not meet the minimum physical activity recommendations. Nowadays, ACC/AHA guidelines in the primary prevention of cardiovascular disease stated that exercise is vital.
Stress management
Wellness promotion, including yoga, meditation, and practicing mindfulness and their role in risk prevention for CVD, has been studied in more than 1,500 research papers. In fact, the positive associations between these practices include improvements in psychological factors such as anxiety, depression, distress, and perceived stress. Besides, some of these interventions resulted in reduced systolic blood pressure. Despite the effective results, these types of interventions are not figured in any prevention guidelines yet.
Â
Â
Conclusions
The world is changing, and we are in search of new treatments. The functional medicine approach is not about staying away from the medical guidelines. Instead, it is to follow them while empowering the patient. In fact, this empowerment comes from the assessment and awareness of the multiple factors contributing to this “bad†ecosystem. This awareness can also provide a sense of “I need to change this for myself†instead of someone else telling the patient to “do as I say so.†The healing journey is different for everybody, but we need to go through it if we want a change.
As a nutritionist, it is exciting to know that science has brought light to the inflammation topic. Now we know that inflammation can be influenced by many factors, we can treat it on various levels. Another amazing finding is that we are no longer treating hypertension by removing the salt from the table. No, instead we can introduce all kinds of new meals and anti-inflammatory foods to the table to prevent or reverse disease. – Ana Paola RodrÃguez Arciniega, MS
References:
Enos, Reilly T et al. “Influence of dietary saturated fat content on adiposity, macrophage behavior, inflammation, and metabolism: composition matters.â€Â Journal of lipid research vol. 54,1 (2013): 152-63. doi:10.1194/jlr.M030700
Arnett, Donna K, et al. “2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines.†Circulation vol. 140,11 (2019): e596-e646. doi:10.1161/CIR.0000000000000678
Scott-Sheldon, Lori A J et al. “Mindfulness-Based Interventions for Adults with Cardiovascular Disease: A Systematic Review and Meta-Analysis.â€Â Annals of behavioral medicine: a publication of the Society of Behavioral Medicine vol. 54,1 (2020): 67-73. doi:10.1093/abm/kaz020
Additional Online Links & Resources (Available 24/7)


Online Appointments or Consultations:Â bit.ly/Book-Online-Appointment
Online Physical Injury / Accident Intake Form: bit.ly/Fill-Out-Your-Online-History
Online Functional Medicine Assessment: bit.ly/functionmed
Disclaimer
The information herein is not intended to replace a one-on-one relationship with a qualified health care professional, licensed physician, and not medical advice. We encourage you to make your own health care decisions based on your research and partnership with a qualified health care professional. Our information scope is limited to chiropractic, musculoskeletal, physical medicines, wellness, sensitive health issues, functional medicine articles, topics, and discussions. We provide and present clinical collaboration with specialists from a wide array of disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the musculoskeletal system’s injuries or disorders. Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and support, directly or indirectly, our clinical scope of practice.* Our office has made a reasonable attempt to provide supportive citations and has identified the relevant research study or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request. We understand that we cover matters that require an additional explanation of how it may assist in a particular care plan or treatment protocol; therefore, to further discuss the subject matter above, please feel free to ask Dr. Alex Jimenez or contact us 915-850-0900.  Read More…
Dr. Alex Jimenez DC, MSACP, CCST, IFMCP*, CIFM*, CTG*
email:Â coach@elpasofunctionalmedicine.com
phone: 915-850-0900
Licensed in Texas & New Mexico
Disclaimers
Professional Scope of Practice *
The information herein on "Cardiometabolic Risk: How to Manage it" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's wellness blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-C) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on dralexjimenez.com, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
