Allergies have been around for what it seems like forever. Most of our patients suffer from environmental or seasonal allergy. Most of the patients with on-going gastrointestinal symptoms self-diagnose with a food allergy, and they start avoiding the food in the matter. Therefore, the exact number of people with a food allergy is unknown, but it’s estimated that the prevalence rate is 3% and less than 10% of adults worldwide.
Several adverse gastrointestinal symptoms, reproducible or not reproducible, can be caused by the ingestion of different foods. Adverse food reactions can be immune derived or non-immune conditions. Food allergy is considered an immune-derived reaction.
Table of Contents
Food allergies: Recent studies had reported that the incidence of food allergy has risen around the globe, but there is no exact number to report. Children’s food allergy prevalence is estimated to be 4% to 7% and 3% to 6% in adults, but the heterogeneity of rates and methodology between studies differs in a large amount. These epidemiological reports are consistent because the proper diagnosis and definition of food allergy are imprecise.
Institute of Allergy and Infectious Diseases defined as food allergy
as ‘‘an adverse health effect arising from a specific immune
response that occurs reproducibly on exposure to a given food’’
Food allergies are adverse immunologic IgE-mediated reactions related to food hypersensitivity. Â The risk factors can be varied:
| Sex (male sex children) | Timing in the exposure to food (weaning) |
| Race/ ethnicity (Asian and black children) | Environmental sensitization |
| Genetics | Obesity |
| Atopy | Inflammatory state |
| Vitamin D deficiency | Probiotics |
| Omega 3 PUFA’s deficiency | |
| Antioxidant deficient diet | |
| Increased hygiene |
The reproducible adverse food reaction called food allergy is associated with the ingestion of different foods, and these can vary depending on the patient’s life stage:
| Childhood (can be resolved) | Adult (persistent) |
| Milk | Peanut |
| Egg | Tree nuts |
| Wheat | Fish |
| Soy | Shellfish |
Diagnose screening:
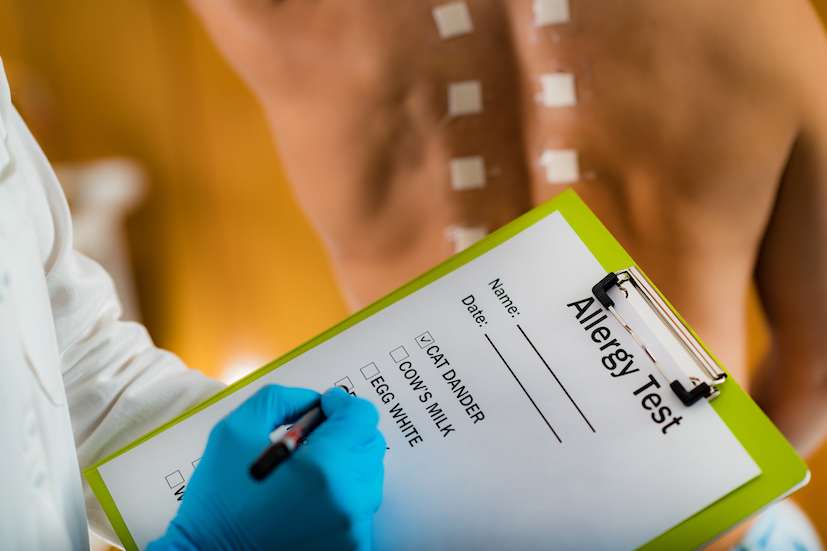
Testing for food allergy can be tricky; false positives or cross-reactions between foods can easily take place. The best approaches are currently regulated by the Expert Panel Guidelines and should be accompanied by a physical examination.
Considered the gold standard.
- Skin Prick Tests
It can be easily reproduced, but cross-reactions to different foods can appear if the test is not properly prepared.
Not appropriate for patients that have a high risk of anaphylaxis or using steroids, antihistamines, dermatitis.
- S IgE measurements
Useful but not diagnostic
- Oral Food Challenges (OFC)
The adverse food reaction should appear within minutes or 2-4 hours after the test. Is considered to be time consuming and risky.
THE CROSS REACTORS |
|||||
| Environmental allergen | Fruits | Vegetables | Nuts | Spices | Other foods |
| Pollen | Apple, cherry, fig, kiwi, lychee, nectarine, pear, plum, peach, apricot. | Beans, carrot, celery, potato, tomato, peas. | Almond, hazelnut, walnut. | Anise, basil, dill, chicory. | Lentils, peanuts, soybean, sunflower. |
| Grass | Date, kiwi, melons, orange, tomato, watermelon. | Peas, potato. | Peanut | ||
| Ragweed | Banana, melons, watermelon. | Cucumbers, Zucchini | |||
An allergy is considered a systemic disease and may be presented with diverse manifestations. Food allergy can have the following adverse reactions.
FOOD ALLERGY MANIFESTATIONS |
|
| DIGESTIVE | NON-DIGESTIVE |
| Immediate gastrointestinal hypersensitivity: IgE mediated reaction, often accompanied by effects in the skin and the lungs. Symptoms:
·      pyloric spams ·      hypotonia ·      vomiting ·      diarrhea |
Cutaneous manifestations:
·      atopic dermatitis ·      urticaria ·      exercise-induced urticaria ·      contact urticaria |
| Oral allergy syndrome: the presence of itching and swelling of oral tissues. | Respiratory:
·    asthma ·      Heiner syndrome ·      coughing or rhinitis |
| Eosinophilic esophagitis and gastritis: IgE mediated and non-IgE mediated, the first involves dysphagia, vomiting, abdominal pain, and irritability. Eosinophilic gastritis is associated with vomiting, abdominal pain, hematemesis, and poor weight gain. | Systemic manifestations: anaphylaxis. |
| Dietary protein enterocolitis: In the first months of life, babies may present vomiting and diarrhea, leading to dehydration. | |
| Celiac disease: an increased transglutaminase activity is found in this disease. | |
| Irritable bowel syndrome and food allergy. | |
Sicherer, Scott H., and Hugh A. Sampson. “Food allergy: epidemiology, pathogenesis, diagnosis, and treatment.” Journal of Allergy and Clinical Immunology 133.2 (2014): 291-307.
Olivier, C. E. “Food allergy.” J Aller Ther S 3 (2013): 2.
Flores Kim, J., et al. “Diagnostic accuracy, risk assessment, and costâ€effectiveness of componentâ€resolved diagnostics for food allergy: a systematic review.” Allergy 73.8 (2018): 1609-1621.
Allergic Living,  Charts, Food Allergy, Fruit & Vegetable  August 30, 2010. www.allergicliving.com/2010/08/30/the-cross-reactors/
Disclaimers
Professional Scope of Practice *
The information herein on "Food Allergy" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's wellness blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-C) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on dralexjimenez.com, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
